News & Events
What Tissue Transglutaminase Antibody IgA Levels Mean for Your Health
You may feel confused or worried when you see your tissue transglutaminase antibody iga results. Many people wonder if high or low tissue transglutaminase antibody iga means something serious. Most individuals with elevated tissue transglutaminase antibody iga do not have celiac disease.
- Only 0.9% of patients with high tissue transglutaminase antibody iga get diagnosed with celiac disease.
Abnormal tissue transglutaminase antibody iga results are rare:
| Study Type | Prevalence of Abnormal IgA Results |
|---|---|
| General Population | 0.3% |
| Certain Cohorts | 1.9% |
| Healthy Controls | 0.3% |
| Juvenile Idiopathic Arthritis Cohorts | Median 1.9% |
You can understand tissue transglutaminase antibody iga more easily if you know these facts. This guide will help you use your results to make smart choices for your health.
Key Takeaways
- High tissue transglutaminase antibody IgA levels suggest a higher risk for celiac disease, but further testing is needed for confirmation.
- Low or normal tTG-IgA levels usually indicate a low chance of celiac disease, reducing the need for invasive procedures like biopsies.
- Borderline tTG-IgA results require follow-up testing to clarify the diagnosis and monitor any changes over time.
- Many conditions, not just celiac disease, can cause elevated tTG-IgA levels, so a comprehensive evaluation is essential.
- Consulting with a healthcare professional is crucial for understanding test results and determining the best next steps for your health.
tTG-IgA Levels & Health
Your tissue transglutaminase antibody IgA (ttg-IgA) levels can give you important clues about your risk for celiac disease and other health conditions. Doctors use this antibody test to help find out if your body reacts to gluten, a protein found in wheat, barley, and rye. The results can be high, low, normal, or borderline. Each result tells a different story about your health.
High tTG-IgA: What It Means
If your ttg-IgA antibody levels are high, you may wonder what this means for your health. High levels of this antibody show a strong link to celiac disease. You have a higher chance of having celiac disease when your ttg antibody is elevated. Doctors see a strong connection between high ttg antibody and the severity of celiac disease. The more your antibody rises, the more damage can happen to your gut lining. This damage is measured by the Marsh grading system, which helps doctors see how much your intestine is affected.
High ttg-IgA antibody levels do not always mean you have celiac disease. You need more tests to confirm the diagnosis. Sometimes, people with high antibody levels do not have symptoms or only have mild problems.
You should know that other diseases can also cause high ttg antibody levels. Here are some conditions linked to elevated ttg-IgA antibody:
- Non-Celiac Gluten Sensitivity (NCGS)
- Wheat Allergy
- Inflammatory Bowel Diseases (IBD)
- Type 1 Diabetes
- Autoimmune Liver Diseases
- Rheumatoid Arthritis
- Thyroid Disorders
- Genetic Conditions
- Casein/Cow’s Milk Intolerance
Doctors use your ttg antibody results along with your symptoms and other tests to decide if you have celiac disease or another disease. If you have high ttg antibody but no symptoms, your risk for celiac disease is lower. In studies of blood donors, only a small number with abnormal ttg antibody were diagnosed with celiac disease. Most people with positive antibody less than three times the upper limit had negative results when retested. Long-term studies show that only a small group with positive ttg antibody develop celiac disease later.
Low or Normal tTG-IgA
Low or normal ttg-IgA antibody levels usually mean you have a low chance of celiac disease. Doctors look at your total IgA and ttg antibody together. If both are normal and your ttg antibody is negative, you probably do not have celiac disease. You may not need a biopsy.
| Total IgA | tTG-IgA Antibody | Probability of Celiac Disease | Need for Biopsy |
|---|---|---|---|
| Normal | Negative | Low | Not needed |
- Negative ttg-IgA antibody results show a decreased risk for celiac disease.
- Most people with normal ttg antibody do not have celiac disease.
- If you have symptoms but your ttg antibody is normal, your doctor may look for other causes.
Borderline tTG-IgA
Sometimes, your ttg-IgA antibody results are borderline. This means your antibody level is close to the cut-off value. You may feel unsure about what to do next. Doctors often repeat the test or order more tests to confirm the result.
- At Rijnstate Hospital, most patients with positive ttg antibody had follow-up tests within 14 months.
- Confirmation tests were done within two months for many children, but fewer adults had quick follow-up.
- Only a small number of patients were retested after a negative ttg antibody result.
- Follow-up testing is important for people at risk for celiac disease. It helps confirm positive results and monitor those who may develop the disease.
If your ttg antibody is borderline, your doctor may ask you to repeat the test or do other antibody tests. You may need a biopsy if your symptoms continue or if your antibody rises over time.
Tip: If you start a gluten-free diet after a celiac disease diagnosis, your ttg-IgA antibody levels should drop. Studies show a 50% decrease in antibody within two months for children. Most patients reach normal antibody levels within six months.
Your ttg-IgA antibody results help guide your next steps. High levels suggest a higher risk for celiac disease, but you need more tests to confirm. Low or normal levels mean a lower risk. Borderline results need follow-up. Always talk to your doctor about your antibody results and what they mean for your health.
What Is Tissue Transglutaminase Antibody IgA?
Role in the Body
You may wonder how tissue transglutaminase antibody IgA works inside your body. This antibody belongs to a group called immunoglobulin a. Your immune system produces immunoglobulin a to help protect your gut and other mucous membranes. When you have celiac disease, your body starts to make tissue transglutaminase antibodies that target an enzyme called transglutaminase. This enzyme helps change gluten into a form that can trigger your immune system.
- Tissue transglutaminase acts as an autoantigen in celiac disease.
- It helps break down gluten peptides, making them more likely to cause an immune reaction.
- Your immune system recognizes transglutaminase as a threat and produces immunoglobulin a antibodies against it.
- These antibodies play a key role in the development of celiac disease.
When your body makes tissue transglutaminase antibody IgA, it shows that your immune system is reacting to gluten. This reaction can damage your gut lining and cause symptoms like stomach pain, diarrhea, and tiredness.
Why Test for tTG-IgA
Doctors use tissue transglutaminase antibody IgA tests to check for celiac disease. This test looks for immunoglobulin a antibodies that target transglutaminase. You may need this test if you have symptoms such as bloating, weight loss, or skin rashes. The test helps your doctor see if your immune system is attacking your own tissues.
- Tissue transglutaminase antibody IgA has a sensitivity of 90–98% and specificity of 95–97%.
- It is the most accurate marker for celiac disease screening.
- In some cases, high levels of tissue transglutaminase antibodies can replace the need for a biopsy, especially in children with strong symptoms.
Your doctor may order this test if you have a family history of celiac disease or other autoimmune conditions. The results help guide further testing and treatment. If your immunoglobulin a levels are low, your doctor may use other tests to check for celiac disease.
Tip: Always eat gluten before testing for tissue transglutaminase antibody IgA. Stopping gluten can lower your immunoglobulin a levels and affect your results.
tTG-IgA Test for Celiac Disease

Screening for Celiac
You may hear about screening for celiac disease if you have stomach pain, diarrhea, or other clinical symptoms. Doctors use the tissue transglutaminase antibody IgA test as the preferred screening tool. This test helps find people who might have celiac disease before they get very sick. Screening works best when you have clinical signs or a family history of celiac. You may need screening if you have unexplained weight loss, skin rashes, or tiredness. Doctors use screening to catch celiac early and prevent long-term problems.
Screening for celiac disease often starts with the tTG-IgA test. You may need more clinical testing if your results are positive or borderline. Screening helps doctors decide if you need a biopsy or other clinical tests for a final diagnosis.
Sensitivity and Accuracy
You want a screening test that gives reliable results. The tTG-IgA test shows high sensitivity and specificity for celiac disease. Sensitivity means the test finds most people with celiac. Specificity means the test does not give many false positives. Here is what studies show about the tTG-IgA test:
- Sensitivity: 85% (23 out of 27 celiac cases were seropositive)
- Specificity: 97% (2 out of 65 controls and one blood donor showed low titre positivity)
Doctors trust the tTG-IgA test for screening because it finds most celiac cases. The EMA-IgA test also shows sensitivity and specificity above 95%. Some reviews say EMA-IgA may be more accurate than tTG-IgA, but tTG-IgA remains the main screening test. You should know that no screening test is perfect. Clinical findings and other tests help confirm the initial diagnosis.
When More Tests Are Needed
Sometimes, screening does not give a clear answer. You may need more clinical testing if your tTG-IgA test is positive, borderline, or if you have strong clinical symptoms. Doctors use other tests and biopsies to make a final diagnosis. Here is a table showing when you need more clinical tests:
| Clinical Scenario | Recommended Follow-Up Tests |
|---|---|
| Suspicion of celiac disease based on clinical signs and symptoms | Anti-endomysial antibodies, small bowel biopsy for definitive diagnosis |
You may need a biopsy if your screening test is positive and you have clinical symptoms. Biopsies remain the gold standard for celiac diagnosis. Doctors use all clinical information, screening results, and other tests to make the best decision for your health.
Tip: Always talk to your doctor about your screening results. You may need more clinical testing for a complete diagnosis.
Interpreting tTG Results

Positive tTG-IgA
When you see a positive tTG-IgA result, you may feel anxious. This result often points to a possible diagnosis of celiac disease or dermatitis herpetiformis. Your doctor looks at your iga level and your symptoms together. If your iga is moderately or strongly positive, you may need a small intestinal biopsy. This test checks for damage in your gut lining. You should know that starting a gluten-free diet can lower your iga. Doctors use this drop in iga to see if your treatment works.
Here is a table that helps you understand what your positive tTG-IgA means:
| Evidence Type | Description |
|---|---|
| Positive tTG-IgA | Indicates a potential diagnosis of celiac disease or dermatitis herpetiformis |
| Moderately to Strongly Positive | May require a small intestinal biopsy for confirmation |
| Negative tTG-IgA | Suggests a decreased likelihood of celiac disease |
| Gluten-Free Diet Impact | Antibody levels may decrease after starting a gluten-free diet |
You should always talk to your doctor about your iga and your symptoms. Your doctor may order more tests to confirm your diagnosis.
Negative tTG-IgA
A negative tTG-IgA result usually means you have a low chance of celiac disease. You may feel relieved when you see a negative iga. Doctors use this result to rule out celiac disease. Sometimes, you may have symptoms but still get a negative iga. This can happen for several reasons:
- Selective iga deficiency is common and can lead to negative tTG-IgA results even if you have celiac disease symptoms.
- False negatives can occur with the tTG-IgA test. The sensitivity may be as low as 35.4%, so the test may not work for everyone.
- Other conditions may cause symptoms that look like celiac disease.
If you have symptoms and a negative iga, your doctor may check your total iga. You may need other tests to find the cause of your symptoms.
Indeterminate Results
Sometimes, your tTG-IgA results are not clear. You may see a borderline or indeterminate result. This means your iga is close to the cut-off value. You may feel confused about what to do next. Doctors often repeat the test or use other antibody tests. You may need a biopsy if your symptoms continue or if your iga rises over time.
Tip: If your iga is borderline, do not start a gluten-free diet before talking to your doctor. Changing your diet can affect your iga and make it harder to get a clear diagnosis.
You should follow up with your doctor if your results are indeterminate. Your doctor will guide you on the next steps.
Celiac Disease and Other Conditions
Celiac Disease Diagnosis
You may wonder how doctors confirm celiac disease after you get your tissue transglutaminase antibody IgA results. The diagnosis and management of celiac disease starts with your blood test. Doctors look for high levels of this antibody when you eat gluten. If your tTG-IgA is ten times the upper limit, you have a 95% chance of having celiac. The test shows high sensitivity and specificity, which means it finds most people with celiac and rarely gives a false positive.
| Serologic test | Sensitivity (%) | Specificity (%) | Positive Predictive Value |
|---|---|---|---|
| IgA tissue transglutaminase | 95 to 98 | 94 to 95 | 95% (≥ 10x ULN) |
Doctors may also check your symptoms, family history, and sometimes order a biopsy. You need to keep eating gluten before testing. If you stop, your antibody levels may drop and make diagnosis harder. After diagnosis, you start gluten-free eating for healing. Your doctor will guide your diagnosis and management plan.
Other Diseases Linked to tTG-IgA
You may see abnormal tTG-IgA levels even if you do not have celiac. Some autoimmune and gut diseases can cause this. Your doctor checks for these conditions during diagnosis and management. Here are some diseases linked to abnormal tTG-IgA:
- Celiac disease
- Insulin-dependent diabetes mellitus
- Other autoimmune diseases
- Gastro-oesophageal reflux disease (GORD)
- Recurrent abdominal pain
You may need more tests if you have symptoms but do not fit the classic celiac profile. Your doctor uses your history and test results to decide on diagnosis and management. Healing starts when you find the right cause.
Symptoms with Normal tTG-IgA
You may have symptoms even if your tTG-IgA is normal. Some people react to gluten without showing high antibody levels. You might feel sick after eating gluten, but your blood test looks normal. Doctors call this non-celiac gluten sensitivity. You may see symptoms like diarrhea, constipation, anemia, or depression. These symptoms can make diagnosis and management tricky.
| Symptom | Prevalence (%) | Confidence Interval (95% CI) |
|---|---|---|
| Diarrhea | 46 | 36–55 |
| Constipation | 18 | 11–26 |
| Anemia | 26 | 18–35 |
| B12 deficiency | 10 | N/A |
| Depression | 10 | N/A |
| Liver disease | 10 | N/A |
| Type 1 diabetes mellitus | 8 | N/A |
| Thyroid disease | 11 | N/A |
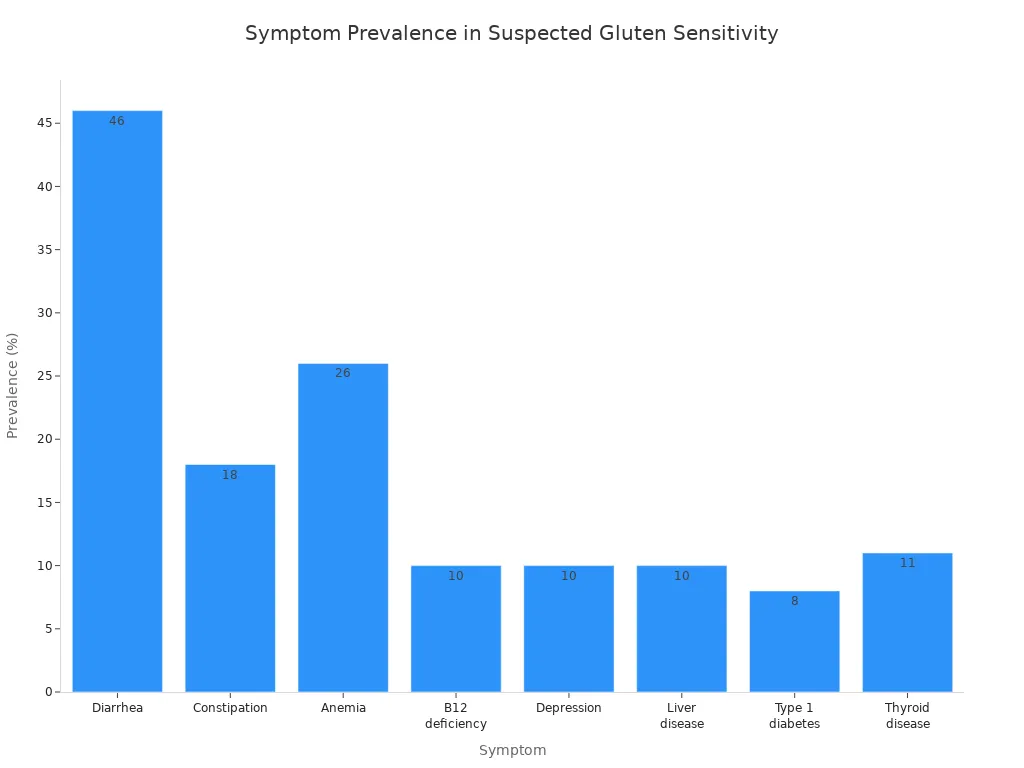
You may need a gluten-free diet for healing, even if you do not have celiac disease. Your doctor will help you with diagnosis and management. You should track your symptoms and see if they improve when you avoid gluten. Healing takes time, but you can feel better with the right plan.
Next Steps After Your Test
When to See a Specialist
You may feel unsure about what to do after your tissue transglutaminase antibody IgA testing. Seeing a specialist can help you understand your results and plan your next steps. You should see a gastroenterologist if:
- You have abnormal celiac serology or symptoms that suggest celiac disease while you still eat gluten.
- Your abnormal celiac serology continues even after you have followed a gluten-free diet for over a year.
- You find it hard to follow a gluten-free diet or need more education about your diet.
- You have celiac disease and other health problems that make it hard to manage your diet.
A specialist can guide you through more testing and help you manage your health. You do not need to wait if you have ongoing symptoms or trouble with your diet.
Additional Testing
After your first testing, your doctor may recommend more testing to confirm your diagnosis. The type of testing depends on your results and symptoms. Here is a table that shows common follow-up tests:
| Test Recommendation | Description |
|---|---|
| Small Intestinal Biopsy | Confirmatory test for celiac disease diagnosis in individuals with positive tTG IgA results. |
| Endomysial Antibody (EMA) IgA Testing | Recommended for tTG IgA concentrations between 5 FLU and 10 FLU to improve positive predictive value. |
| Monitoring tTG IgA Levels Post-Diet Change | A decrease in tTG IgA levels after starting a gluten-free diet indicates a positive response to therapy. |
Your doctor may repeat testing to see if your antibody levels change over time. You may need a biopsy to check your gut if your testing stays positive. Testing helps your doctor track your progress and adjust your treatment plan.
Diet and Lifestyle
If your testing shows celiac disease, you need to make changes to your diet and lifestyle. You must avoid gluten to protect your health. Here are some important steps:
- Avoid grains like wheat, barley, and rye.
- Stay away from foods such as bread, pasta, breakfast cereals, biscuits, crackers, cakes, pastries, pies, gravies, and sauces.
- Always check food labels to make sure you do not eat gluten by mistake.
You should talk to a dietitian who knows about celiac disease. A dietitian can help you plan meals and teach you how to read labels. You may need to learn new recipes and find safe foods. A gluten-free diet is the only way to heal your gut and prevent future problems. You can still enjoy many foods and live a healthy life with the right support.
Tip: Keep a food diary to track what you eat and how you feel. This can help you and your doctor see how your diet affects your symptoms.
Common Misconceptions
False Positives and Negatives
You may think tissue transglutaminase antibody IgA testing always gives a clear answer. This is not true. Sometimes, you can get a false positive or false negative result. Hemolysis, which happens when red blood cells break during blood collection, can change your test results. This can make your antibody levels look higher or lower than they really are.
Many conditions can cause false positives. Autoimmune diseases, non-autoimmune cirrhosis, linear IgA dermatosis, herpes gestationis, and vasculitis can all affect your test. In one study, 6.1% of patients with high IgM rheumatoid factor had false-positive anti TG2 antibodies.
False negatives can also happen. If you have selective IgA deficiency, your body does not make enough IgA. This can cause your test to miss celiac disease. Some patients with celiac disease test negative for tTG antibodies but still have the disease. Anti-gliadin antibodies (AGAs) can show celiac disease even when tTG is negative, but doctors often overlook this.
Always talk to your doctor about your symptoms and test results. One test alone cannot give you the full picture.
Common misconceptions about tTG-IgA testing:
- You can have celiac disease even if your tTG-IgA test is negative.
- Selective IgA deficiency can cause false negatives.
- Anti-gliadin antibodies may help diagnose celiac disease when tTG-IgA is negative.
Non-Celiac Causes
You may believe only celiac disease causes high tTG-IgA levels. This is a common mistake. Many other conditions can raise your antibody levels. Autoimmune diseases, liver problems, and skin disorders can all affect your test. Hemolysis during blood collection can also change your results.
Conditions linked to false positive tTG-IgA results:
- Autoimmune diseases
- Non-autoimmune cirrhosis
- Linear IgA dermatosis
- Herpes gestationis
- Vasculitis
You should know that high tTG-IgA does not always mean you have celiac disease. Your doctor looks at your symptoms, history, and other tests before making a diagnosis.
Test Limitations
No test is perfect. Tissue transglutaminase antibody IgA testing has some limits you need to know. Selective IgA deficiency happens more often in people with celiac disease than in the general population. This can lead to false negatives. Young children under two years old may test negative for anti-endomysial antibodies, which makes diagnosis harder. If you have selective IgA deficiency, your doctor may check IgG antibodies instead.
| Limitation | Description |
|---|---|
| Selective IgA Deficiency | Happens 10- to 16-fold more often in celiac patients. Causes false negatives. |
| Age Factor | Children under 2 years may test negative for anti-endomysial antibodies. |
| Alternative Antibodies | IgG antibodies may be high in selective IgA deficiency. IgG-EmA testing helps. |
You should remember that your doctor uses more than one test to diagnose celiac disease. Your symptoms, history, and other lab results all matter.
Understanding your tTG-IgA results helps you take control of your health.
- The tTG-IgA test is the gold standard for celiac disease screening.
- High levels often mean a strong chance of celiac disease, especially if you have symptoms.
- Knowing your results can help you avoid serious health risks and improve long-term outcomes.
| Follow-Up Steps | Details |
|---|---|
| Referral to Dietitian | Meet with a dietitian for guidance and support. |
| Dietary Interview | Check how well you follow a gluten-free diet. |
| Serology Testing | Repeat tTG-IgA testing as needed. |
| Lab Tests | Monitor for vitamin and mineral problems. |
| Regular Follow-Up | See your doctor every 3-6 months, then once or twice a year. |
Always talk to your doctor about your results. Abnormal results do not mean you have celiac disease for sure. Follow-up testing and specialist care can help you find answers and protect your health.
FAQ
What does a high tTG-IgA level mean for you?
High tTG-IgA levels suggest a strong chance of celiac disease. You may need more tests to confirm. Some autoimmune diseases can also cause high levels. Your doctor will help you understand your results.
Can you have celiac disease with a normal tTG-IgA result?
Yes, you can. Selective IgA deficiency or testing too early may cause a normal result. If you have symptoms, your doctor may order more tests. Always share your symptoms with your doctor.
Should you stop eating gluten before the tTG-IgA test?
No, you should not stop eating gluten before testing. Stopping gluten can lower your antibody levels. This may lead to a false negative result. Keep eating gluten until your doctor tells you otherwise.
What other conditions can raise tTG-IgA levels?
Autoimmune diseases, liver problems, and skin disorders can raise tTG-IgA levels.
Your doctor will check your history and symptoms before making a diagnosis.
How often should you repeat tTG-IgA testing?
You should repeat tTG-IgA testing every 3 to 6 months after starting a gluten-free diet. Your doctor may adjust this based on your symptoms and progress. Regular testing helps track your healing.