News & Events
Gliadin Antibody or tTG-IgA Which Test Wins

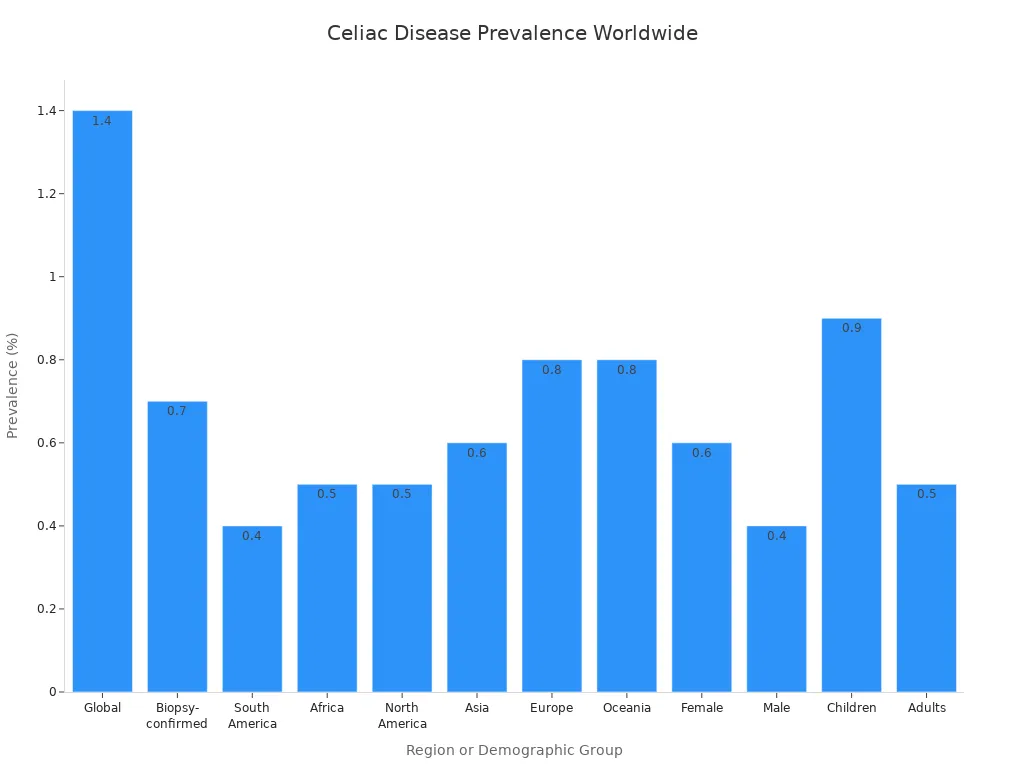
Do you wonder which test gives you the most accurate diagnosis of celiac disease? Most doctors choose tTG-IgA, but the gliadin antibody test, especially when using deamidated gliadin, still matters. You need to know the differences because the right test can help detect celiac early and prevent long-term disease effects. Celiac affects people worldwide, with a global prevalence of about 1.4%.
Learning which test to ask for can make a difference in your diagnosis and health.
Key Takeaways
- The tTG-IgA test is the gold standard for diagnosing celiac disease due to its high sensitivity and specificity.
- Deamidated gliadin peptide (DGP) tests are more accurate than conventional gliadin tests and are useful for infants and those with IgA deficiency.
- Always eat gluten for 2-4 weeks before testing to ensure accurate results; a gluten-free diet can lead to false negatives.
- If you have symptoms or a family history of celiac, discuss serologic tests with your doctor to get the right diagnosis.
- A positive blood test suggests celiac disease, but a biopsy is needed for a definitive diagnosis.
Gliadin Antibody Testing

Conventional vs. Deamidated Gliadin
When you look at gliadin antibody testing, you will find two main types: conventional gliadin antibody and deamidated gliadin peptide (DGP) antibody. The conventional gliadin antibody test checks for antibodies your body makes against gliadin, a protein found in wheat. This test was common in the past, but it does not work as well for detecting celiac. It often gives false results and misses many cases.
Deamidated gliadin antibodies offer a better choice. These antibodies target gliadin that has changed through a process called deamidation. In celiac, your body’s enzyme, tissue transglutaminase 2 (TG2), changes gliadin. This change helps your immune system recognize the protein more easily, which leads to a stronger and more specific response. The DGP test can find these antibodies with high accuracy.
Tip: Deamidated gliadin peptide tests show much higher sensitivity and specificity than conventional gliadin antibody tests. You can see this in the table below:
| Test Type | Sensitivity | Specificity |
|---|---|---|
| Deamidated Gliadin Peptide Test | 91% | 98% |
| Conventional Gliadin Antibody Test | Low | Low |
Role in Celiac Disease
You might wonder why gliadin antibody tests matter for celiac. These tests work by finding antibodies in your blood that form when your body reacts to gluten. In celiac, your immune system attacks gluten, especially after TG2 changes the gliadin. This process makes the immune response stronger and easier to detect.
Deamidated gliadin antibodies are especially helpful for certain groups. For example, doctors often use the DGP test for infants and young children. If you have IgA deficiency, which is more common in people with celiac, the DGP-IgG test can help. This test does not rely only on IgA, so it can still find the disease even if your IgA levels are low.
| Patient Population | Preferred Testing Method |
|---|---|
| Infants and Young Children | Deamidated Gliadin Peptide Antibodies |
| Patients with IgA Deficiency | DGP-IgG Test |
You should know that while the DGP test is very accurate, doctors usually use it when tTG-IgA is not enough or when special situations arise. Still, it plays a key role in making sure you get the right diagnosis.
tTG-IgA and Celiac Diagnosis
How tTG-IgA Works
You might wonder how the tTG-IgA test helps doctors find celiac. Tissue transglutaminase, or tTG, is an enzyme in your body. When you eat gluten, tTG interacts with parts of gluten called gliadin peptides. This process forms complexes that your immune system can see as a threat. Your body then makes IgA antibodies against tTG. These antibodies show up in your blood if you have celiac.
- tTG is the main autoantigen in celiac.
- The immune system reacts to tTG and gliadin complexes.
- IgA antibodies against tTG signal an autoimmune response.
- The tTG-IgA test uses enzyme immunoassay (EIA) to measure these antibodies.
- You need to eat gluten for the test to work well.
Doctors use this test because it is sensitive and specific. If you have enough IgA, the tTG-IgA test can find celiac in most people. If you have IgA deficiency, doctors may use a different test that looks for IgG antibodies.
Why It’s the Gold Standard
You want a test that gives clear answers. The tTG-IgA test stands out for its accuracy and ease of use. Most experts call it the gold standard for the diagnosis of celiac disease. It works well for routine detection and helps doctors decide if you need a biopsy.
| Characteristic | tTG-IgA |
|---|---|
| Sensitivity | 98% |
| Specificity | 98% |
| Ease of Use | Widely available and easy to perform |
| Cost-Effectiveness | Less expensive than other tests |
| Diagnostic Accuracy | Improved with human tTG |
| False Positives | Unusual with human substrates |
The test shows high sensitivity and specificity, which means it finds most people with celiac and rarely gives a false positive. In biopsy-proven celiac patients, tTG-IgA levels are almost always high. The chart below shows how sensitivity and specificity can change with different IgA levels and test cutoffs:
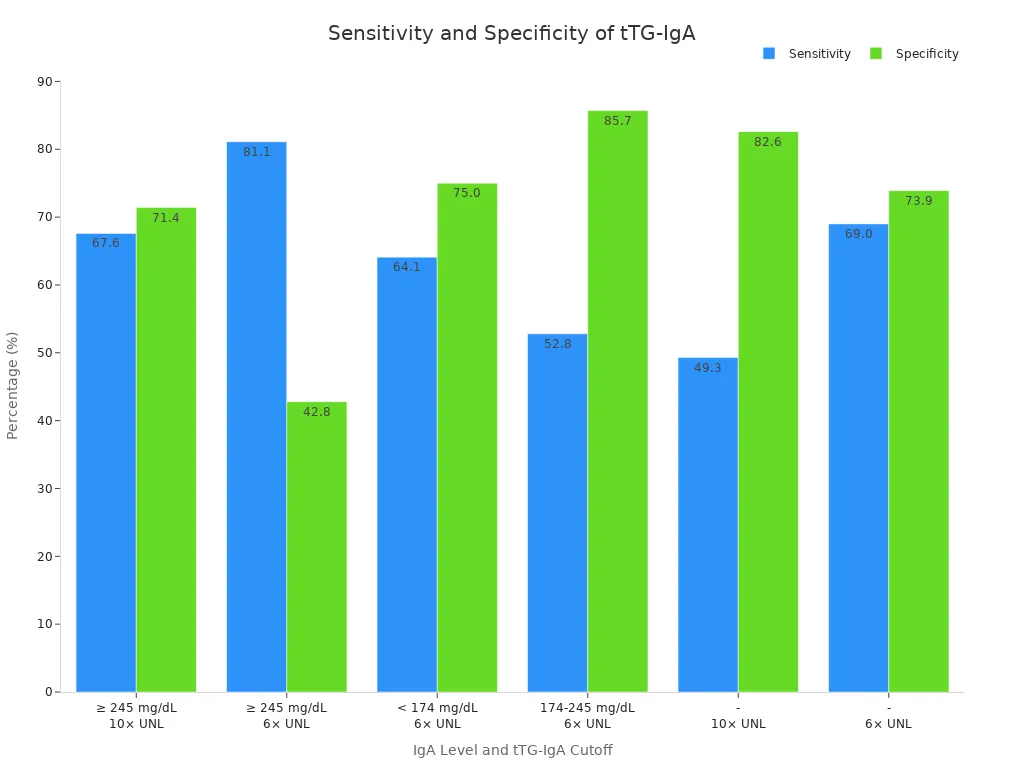
Doctors trust this test because it is simple, cost-effective, and reliable. You can feel confident that the tTG-IgA test will help your doctor make the right diagnosis and guide you toward better health if you have celiac disease.
Test Comparison for Detection of Celiac Disease

Accuracy and Reliability
You want a test that gives you clear answers about celiac. The two main serologic tests for celiac disease are tTG-IgA and deamidated gliadin peptide (DGP) antibodies. Each test has different sensitivity and specificity, which measure how well the test finds the disease and avoids false alarms.
- tTG-IgA shows higher sensitivity than DGP-IgA and DGP-IgG. This means tTG-IgA finds more people who truly have celiac.
- The specificity of tTG-IgA is lower than DGP-IgG, but it still performs well in most cases.
- DGP-IgG has perfect specificity in some studies, so it almost never gives a false positive, but its sensitivity is lower than tTG-IgA.
Here is a quick look at how these tests compare:
| Test Type | Sensitivity (%) | Specificity (%) |
|---|---|---|
| tTG-IgA | 90-98 | 95-97 |
| DGP-IgA | 62.7 | — |
| DGP-IgG | 80.4 | 100 |
| AGA IgA | 80-90 | 85-95 |
| AGA IgG | 75-85 | 75-90 |
You can see that tTG-IgA stands out for its diagnostic accuracy. Most experts consider it the best serologic test for celiac disease screening. DGP-IgG can help in special cases, but isolated positive DGP-IgG results may not always mean you have celiac.
When to Use Each Test
You may wonder when to choose one test over another. Doctors usually start with tTG-IgA because it works well for most people. This test is the preferred diagnostic test for celiac, according to major guidelines.
| Scenario | Best Test(s) |
|---|---|
| First-line screening for celiac | tTG-IgA |
| Suspected celiac with IgA deficiency | DGP-IgG or tTG-IgG |
| Inconclusive tTG-IgA results | DGP antibody testing as a reflex test |
| Infants and young children | DGP antibody testing may be considered |
| Confirming diagnosis in biopsy-proven celiac patients | tTG-IgA |
- You should use tTG-IgA as your first step in the detection of celiac disease.
- If you have IgA deficiency, your doctor may order DGP-IgG or tTG-IgG.
- DGP antibody testing is not the first choice but can help when tTG-IgA results are unclear.
- Gliadin antibody tests are no longer recommended as the main test for diagnosis.
Note: The American College of Gastroenterology and other experts recommend tTG-IgA as the best first test for suspected celiac. You still need a biopsy to confirm the diagnosis if your serologic tests are positive.
Limitations and False Results
No test is perfect. Both tTG-IgA and DGP antibody tests have some limitations and can give false results.
| Test Type | False Negatives | False Positives |
|---|---|---|
| tTG IgA | 28 | 112 |
| DGP IgG | 5 | 207 |
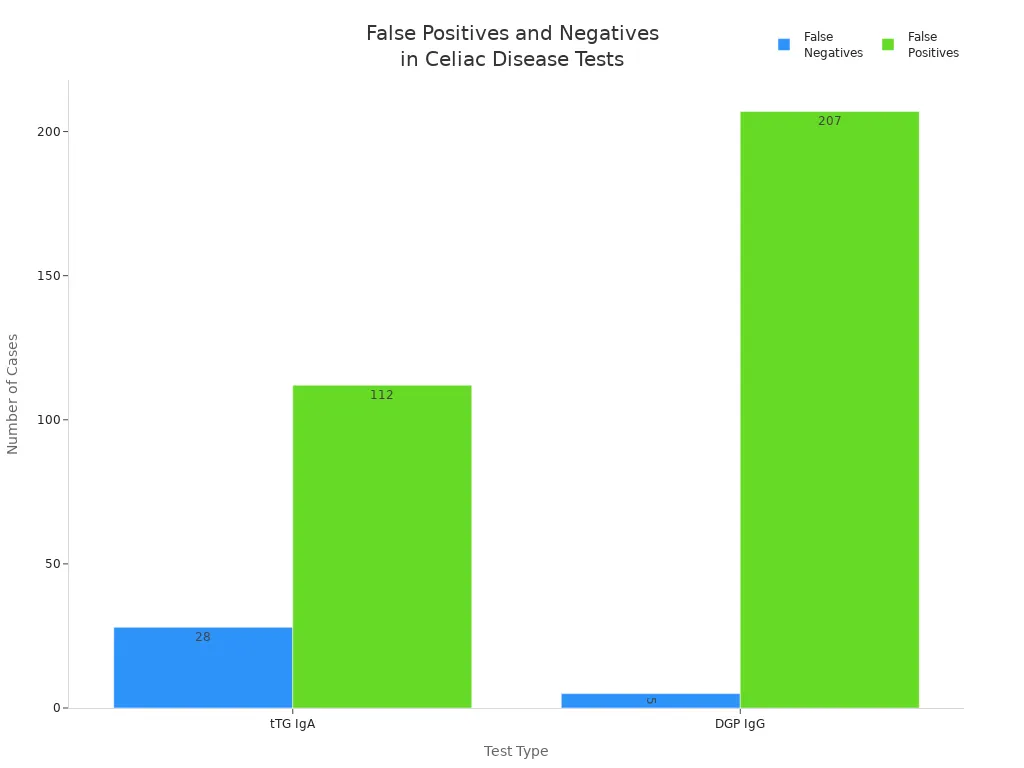
- tTG-IgA can give false positives, especially in people with other autoimmune diseases.
- DGP-IgG can give more false positives than tTG-IgA, which may lead to extra testing.
- Both tests can give false negatives if you have already stopped eating gluten.
- A positive serologic test suggests celiac, but you still need a biopsy to confirm the disease.
| Limitation | Description |
|---|---|
| Non-conclusiveness | A positive antibody test suggests celiac but requires a biopsy for certainty |
| Diet Dependency | Tests work best when you eat gluten; a gluten-free diet can affect results |
If you have IgA deficiency, serologic tests for celiac disease may not work as well. In this case, your doctor may use IgG-based tests or go straight to a biopsy. About 0.75% of people tested for IgA deficiency actually have it, and only some of them get a proper diagnosis with biopsy or IgG-tTG.
You should always talk to your doctor about your symptoms, diet, and test results. This helps you get the right diagnosis and avoid unnecessary worry.
Expert Recommendations for Disease Testing
Guidelines and Best Practices
You want the best chance at an accurate diagnosis when you suspect celiac. Major gastroenterology societies agree that the serum IgA anti-tissue transglutaminase antibody, also called the iga anti-ttg test, is the first-line diagnostic test for celiac. You should take this test while you still eat gluten, because stopping gluten can affect your results. Experts recommend measuring total serum iga at the same time. This step helps find people with iga deficiency, which can cause false negatives.
International guidelines show some differences in their approach. Here is a quick look:
| Guideline | Recommended Test | Notes |
|---|---|---|
| ESPGHAN | tTG-IgA | Initial testing with tTG-IgA and total IgA combined |
| NASPGHAN | tTG-IgA + DGP IgG | Combined use to improve diagnostic accuracy |
| ACG | tTG-IgA + DGP IgG | Combined use to improve diagnostic accuracy |
| General | AGA test | Not recommended due to low diagnostic accuracy |
For children under 2 years old, you should ask for both the DGP antibody and tTG-IgA tests. This approach improves detection of celiac disease in young children, where the sensitivity of tTG-IgA alone may be lower. Experts do not recommend the iga anti-native gliadin antibodies test anymore, because it does not have good diagnostic performance.
Tip: Always use serologic tests for celiac disease while eating gluten. Blood tests are not reliable if you have already stopped gluten.
Advice for Patients
You can take steps to get the most accurate results. Stay on a gluten-containing diet before testing. If you have symptoms like stomach pain, diarrhea, or a family history of celiac, ask your doctor about serologic tests. The tTG-IgA test is the best starting point for most people. If you have iga deficiency or are under 2 years old, your doctor may add the DGP antibody test.
- Remain on a gluten diet for at least 2-4 weeks before testing.
- Ask your doctor to check total serum iga to rule out deficiency.
- Remember, a negative tTG-IgA test does not always rule out celiac, especially if you have symptoms.
- If you have risk factors like autoimmune disease or a family history, discuss further testing.
You should know that the gliadin antibody test is not the main test anymore. The best serologic tests for celiac disease focus on tTG-IgA and DGP antibodies. These tests have high sensitivity and specificity, which means they give you the most reliable results. If you have questions about your results or which test to choose, talk with your healthcare provider. You can help guide your care by understanding the differences in diagnostic accuracy and performance.
You want the most accurate test for celiac. The tTG-IgA test stands out because it offers high sensitivity and specificity, as shown below:
| Metric | Value |
|---|---|
| Sensitivity | > 90% |
| Specificity | > 95% |
| Positive Predictive Value | 89.4% |
| Negative Predictive Value | 99.0% |
In special cases, like young children or those with IgA deficiency, deamidated gliadin peptide antibody testing helps doctors find the disease early. Talk with your healthcare provider about the best testing option for you. Early and accurate detection can improve your quality of life and help you manage your health with confidence.
FAQ
What is the main difference between tTG-IgA and gliadin antibody tests?
tTG-IgA checks for antibodies against tissue transglutaminase. Gliadin antibody tests look for antibodies against gluten proteins. tTG-IgA gives more accurate results for most people.
Can you take these tests if you already eat gluten-free?
You need to eat gluten for a few weeks before testing. Gluten-free diets can cause false negatives. Ask your doctor how long you should eat gluten before testing.
Why do doctors sometimes order both tTG-IgA and DGP tests?
Doctors order both tests if you are under 2 years old or have IgA deficiency. This approach helps find celiac disease in special cases.
Are these blood tests enough to diagnose celiac disease?
You need a biopsy to confirm celiac disease. Blood tests help screen for the disease, but a biopsy of your small intestine gives a definite answer.
What should you do if your test results are unclear?
- Talk to your doctor.
- Ask about repeat testing or a biopsy.
- Share your symptoms and family history.
Your doctor can guide you to the next steps for a clear diagnosis.

