News & Events
A Guide to Anti Centromere Antibody and Its Role in Autoimmune Disorders
You may have heard about the anti centromere antibody if you or someone you know faces questions about autoimmune diseases. This antibody targets a part of your cell’s nucleus. Doctors often use the anti-centromere antibody test to help diagnose certain conditions. About one-third of people with systemic sclerosis test positive for anti-centromere antibodies, with most showing the limited type, including crest syndrome. You can also find anti-centromere in other conditions like primary biliary cirrhosis, Sjögren’s syndrome, and rheumatoid arthritis, though less often.
Key Takeaways
- The anti-centromere antibody test is crucial for diagnosing autoimmune diseases like systemic sclerosis and CREST syndrome. A positive result indicates a high likelihood of these conditions.
- Understanding the role of anti-centromere antibodies can help you recognize symptoms early. Symptoms like Raynaud’s phenomenon and skin changes may signal the need for testing.
- If your doctor orders the anti-centromere antibody test, ask about the clinical significance of your results. This can guide your treatment and management plan.
- A positive test result does not guarantee serious disease. Your doctor will consider your symptoms and other findings to determine the best next steps.
- Regular communication with healthcare providers is essential. They can help you understand your risk and manage symptoms effectively.
Anti Centromere Antibody Overview
What Are Anti-Centromere Antibodies?
You may wonder what makes the anti centromere antibody so important in the world of autoimmune diseases. This autoantibody targets specific proteins found in the centromere, a key part of your cell’s nucleus. The centromere acts as the anchor point for chromosomes during cell division. When your immune system creates anti-centromere antibodies, it mistakes these centromere proteins for threats.
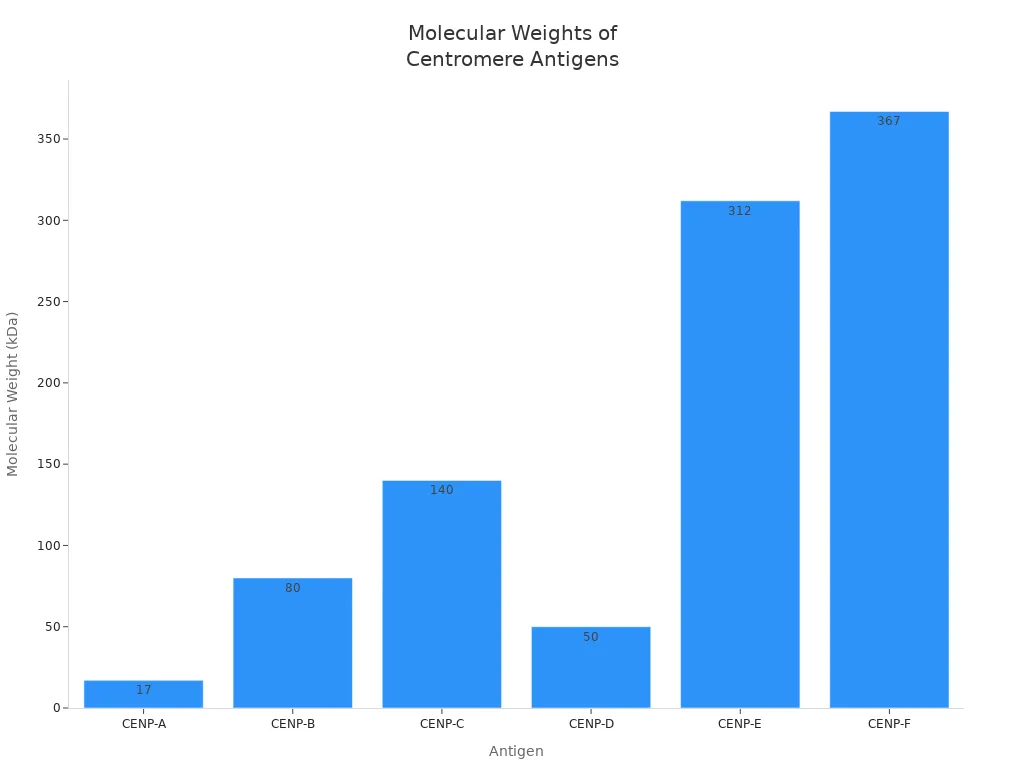
Scientists have identified several centromere proteins that these autoantibodies can target. Each protein has a unique role in the cell. You can see the main centromere antigens and their features in the table below:
| Antigen | Molecular Weight | Function |
|---|---|---|
| CENP-A | 17kDa | Histone H3-like protein |
| CENP-B | 80kDa | DNA binding protein involved in heterochromatin folding |
| CENP-C | 140kDa | Involved in kinetochore assembly |
| CENP-D | 50kDa | Protein of unknown function, possibly involved in chromatin condensation |
| CENP-E | 312kDa | Kinesin motor protein |
| CENP-F | 367kDa | Associates with the kinetochore in late G2 phase during mitosis |
Note: The centromere contains many proteins, but CENP-A, CENP-B, and CENP-C are the most common targets for the anti centromere antibody.
You may also see a chart that shows the molecular weights of these centromere antigens:
Doctors use different methods for autoantibody detection. The most common ways include indirect immunofluorescence (IIF) and solid-phase immunoassays. These tests help you and your healthcare team find out if you have anti-centromere antibodies in your blood. Patient selection before testing is important because the clinical characteristics of each autoimmune disease can affect the results.
You may hear about different subtypes of anti centromere antibody. For example, ACA-positive Sjögren’s syndrome is a recognized subtype. People with this subtype may show clinical characteristics such as Raynaud’s phenomenon, sclerodactyly, and extraglandular dysfunction. The clinical significance of anti centromere antibody in Sjögren’s syndrome is still not fully understood. However, doctors know that the presence of this autoantibody can help identify certain clinical patterns.
Role in the Immune System
Your immune system usually protects you from germs. Sometimes, it makes a mistake and creates an autoantibody that attacks your own body. The anti centromere antibody is one of these autoantibodies. It targets the centromere–kinetochore macrocomplex, which is a group of proteins that help chromosomes move during cell division.
Researchers have found that in some autoimmune diseases, such as systemic sclerosis, Sjögren’s syndrome, and primary biliary cholangitis, the autoantibody response focuses on the centromere. In Sjögren’s syndrome, antibody-secreting cells often target kinetochore antigens more than CENP-B. This pattern shows that the clinical characteristics of each disease can affect which centromere proteins the autoantibody attacks.
The clinical significance of anti centromere antibody depends on the disease. In systemic sclerosis, the presence of this autoantibody often points to the limited cutaneous form, which has different clinical characteristics than the diffuse form. In primary biliary cholangitis, the anti centromere antibody can appear with other autoantibodies and may signal a higher risk for certain clinical complications.
You should know that the clinical significance of anti centromere antibody is not the same in every disease. Doctors look at the clinical characteristics, the type of autoantibody, and the pattern of centromere protein targeting to decide what the test results mean for you. This careful approach helps you get the right diagnosis and treatment.
Tip: If your doctor orders an anti centromere antibody test, ask about the clinical significance of your results. The meaning can change based on your symptoms and the clinical characteristics of your condition.
Anti-Centromere Antibody Test
Purpose of the Test
You may wonder why your doctor recommends the anti-centromere antibody test. This test acts as a powerful diagnostic tool for identifying certain autoimmune diseases. Doctors use this test to look for specific antibodies in your blood that target the centromere, a part of your cell’s nucleus. The anti-centromere antibody test helps you and your healthcare team find out if your immune system is attacking your own body.
The main purpose of the anti-centromere antibody test is to help with the diagnosis of limited cutaneous systemic sclerosis, also known as CREST syndrome. This test stands out as a highly specific diagnostic tool for this condition. In fact, the anti-centromere antibody test has a specificity of over 97% for systemic sclerosis. This means that if you test positive, you have a high chance of having this disease. The test also helps doctors separate limited cutaneous systemic sclerosis from other types of autoimmune diseases.
You may also see the anti-centromere antibody test used as a diagnostic tool for other autoimmune conditions. These include primary biliary cholangitis, Sjögren’s syndrome, rheumatoid arthritis, and systemic lupus erythematosus. The test can even predict the risk of developing systemic sclerosis years before symptoms appear. If you have Raynaud’s phenomenon, your doctor may use this test to check your risk for systemic sclerosis.
Doctors often look at the titer, or concentration, of antibodies in your blood. A higher titer, such as 1:1280, usually means a stronger immune response. The titer helps your doctor decide how likely it is that you have a specific autoimmune disease. The anti-centromere antibody test, as a diagnostic tool, gives your doctor important information about your risk and helps guide your treatment plan.
You can see how the anti-centromere antibody test performs in different groups in the table below:
| Condition | Sensitivity (%) | Specificity (%) |
|---|---|---|
| Normal controls | 33 | 99.9 |
| Other connective tissue diseases | 31 | 95-97 |
| Primary Raynaud’s phenomenon | 24 | 90 |
| Non-SSc relatives | 19 | >99 |
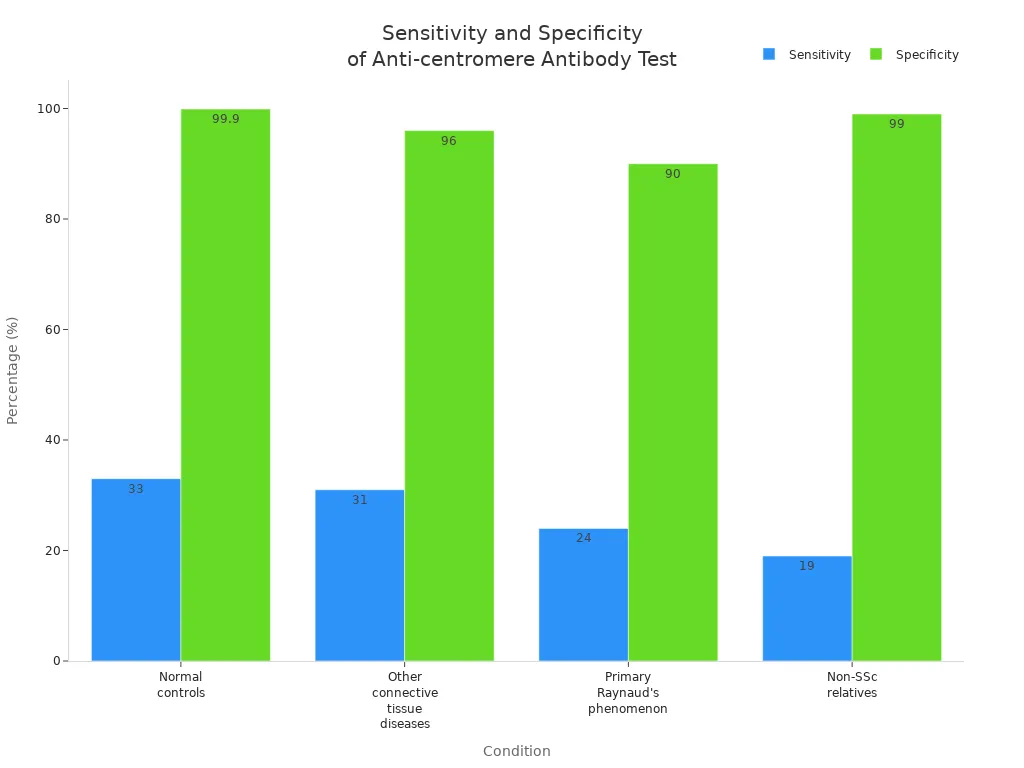
Note: The anti-centromere antibody test is a diagnostic tool with high specificity but moderate sensitivity. A positive test result is very helpful for diagnosis, but a negative test does not rule out disease.
When Is the Test Ordered?
Doctors order the anti-centromere antibody test when you show signs or symptoms that suggest an autoimmune disease. This test is a key diagnostic tool for diagnosing autoimmune diseases, especially when you have symptoms linked to systemic sclerosis or CREST syndrome. The test helps your doctor confirm a diagnosis and decide on the best treatment.
You may need the anti-centromere antibody test if you have:
- Fatigue
- Joint pain
- Skin abnormalities
Doctors also use the anti-centromere antibody test as a diagnostic tool when you have certain clinical features. These features often point to systemic sclerosis or related conditions. The table below shows common clinical scenarios that prompt your doctor to order the test:
| Clinical Scenario | Description |
|---|---|
| Systemic Sclerosis | A serious autoimmune condition affecting the skin and organs. |
| CREST Syndrome | A subset of scleroderma characterized by specific symptoms. |
| Calcinosis | Calcium deposits in the skin. |
| Raynaud’s Phenomenon | Reduced blood flow to extremities. |
| Esophageal Dysfunction | Difficulty swallowing due to esophageal issues. |
| Sclerodactyly | Thickened, tight skin on fingers. |
| Telangiectasia | Small, visible dilated blood vessels on the skin. |
| Persistent Skin Changes | Ongoing alterations in skin texture or appearance. |
| Difficulty Swallowing | Challenges in swallowing food or liquids. |
| Unexplained Circulation Problems | Issues with blood flow that are not easily explained. |
You may also need the anti-centromere antibody test if you have overlap diseases, such as primary biliary cholangitis, rheumatoid arthritis, or Sjögren’s syndrome. The test acts as a diagnostic tool to help your doctor understand your symptoms and make a clear diagnosis.
Doctors use the anti-centromere antibody test as a diagnostic tool in these situations:
- You have Raynaud’s phenomenon and your doctor wants to check your risk for systemic sclerosis.
- You show signs of CREST syndrome, such as calcinosis, Raynaud’s phenomenon, esophageal dysfunction, sclerodactyly, or telangiectasia.
- You have unexplained skin changes or circulation problems.
- You have symptoms that do not fit a single disease, and your doctor suspects an overlap syndrome.
The anti-centromere antibody test helps your doctor decide if you need more tests or if you should start treatment. The test can also help predict your risk of developing systemic sclerosis in the future. The presence of anti-centromere antibodies often appears years before you develop symptoms. This makes the test a valuable diagnostic tool for early detection.
You may wonder how the anti-centromere antibody test compares to other tests. The test is highly specific for systemic sclerosis, especially the limited cutaneous form. The test is less sensitive, so not everyone with the disease will test positive. The test can also help your doctor rule out other autoimmune diseases. The anti-centromere antibody test, as a diagnostic tool, gives you and your doctor important information for diagnosis and management.
Tip: If your doctor orders the anti-centromere antibody test, ask about your titer level. A higher titer may mean a stronger immune response and a higher risk for certain diseases.
The anti-centromere antibody test is a key diagnostic tool for diagnosing autoimmune diseases. The test helps your doctor confirm a diagnosis, predict your risk, and guide your treatment. The test is most useful for systemic sclerosis and CREST syndrome, but it can also help with other autoimmune diseases. The test gives you and your doctor the information you need to make the best decisions for your health.
Disease Associations

Systemic Sclerosis and CREST Syndrome
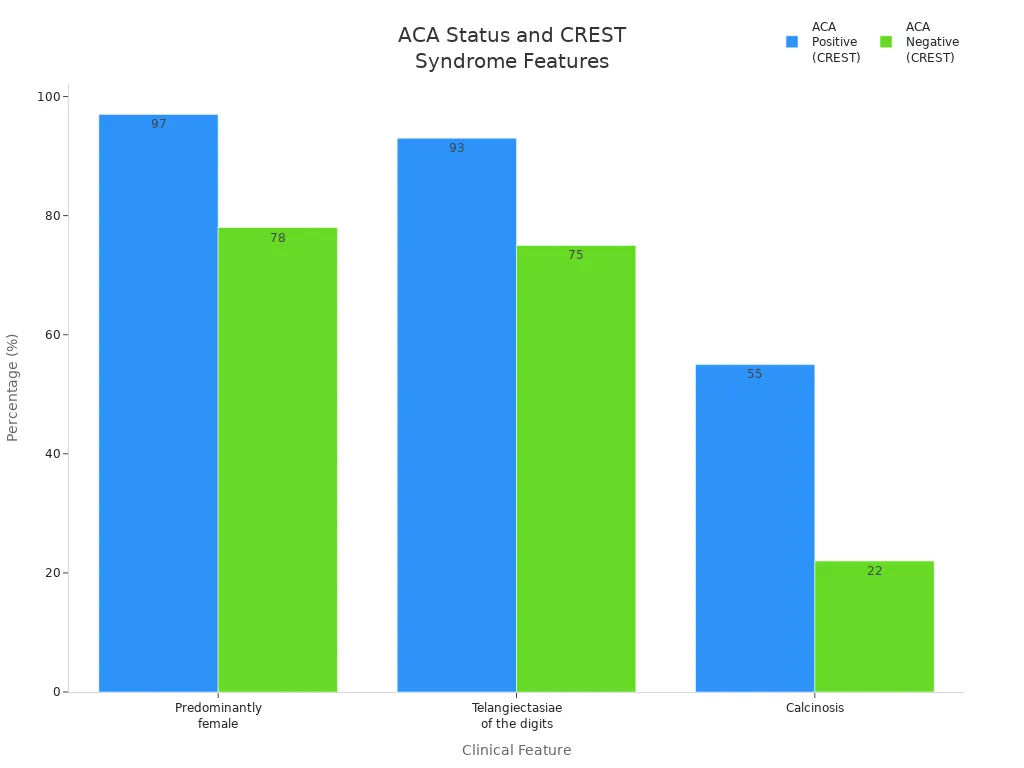
You may notice that scleroderma, especially systemic sclerosis, has a strong link with the anti centromere antibody. Most people with limited cutaneous systemic sclerosis, also called CREST syndrome, show this antibody in their blood. About 82-96% of patients with crest syndrome test positive for anti-centromere. This makes the test very useful for diagnosis. You often see symptoms like raynaud’s phenomenon, sclerodactyly, and skin thickening. These symptoms can appear before other signs of scleroderma. CREST syndrome stands for Calcinosis, Raynaud’s phenomenon, Esophageal dysfunction, Sclerodactyly, and Telangiectasia. You may see more telangiectasia and calcinosis in patients with anti-centromere than those without it. The table below shows how features differ between ACA positive and negative crest syndrome:
| Feature | ACA Positive (CREST) | ACA Negative (CREST) |
|---|---|---|
| Older at onset of symptoms | Yes | No |
| Predominantly female | 97% | 78% |
| Telangiectasiae of the digits | 93% | 75% |
| Calcinosis | 55% | 22% |
| Pulmonary interstitial fibrosis | Less frequent | More frequent |
| Survival difference | No | No |
Sjögren’s Syndrome
You may also find anti-centromere in Sjögren’s syndrome, another chronic autoimmune disease. About 3.7% to 27% of patients with this condition have the antibody in their blood. If you have ACA-positive Sjögren’s syndrome, you may notice more severe symptoms. These include dry mouth, dry eyes, and glandular dysfunction. Studies show that ACA-positive patients often have unique clinical and pathological features. You may need special treatment if you have these symptoms.
| Study Title | Findings |
|---|---|
| Clinical influences of anticentromere antibody on primary Sjögren’s syndrome in a prospective Korean cohort | ACA-seropositive Sjögren’s syndrome shows distinct clinical and pathological features. |
| Association of anticentromere antibodies with more severe exocrine glandular dysfunction in Sjogren’s syndrome | ACA presence correlates with increased severity of glandular dysfunction. |
| A clinical and histopathological analysis of the anti-centromere antibody positive subset of primary Sjogren’s syndrome | Highlights unique clinical and histopathological characteristics in ACA-positive patients. |
| Clinical and immunological features of anti-centromere antibody-positive primary Sjogren’s syndrome | Discusses the immunological implications and clinical features associated with ACA positivity. |
Primary Biliary Cirrhosis
Primary biliary cirrhosis, now called primary biliary cholangitis, is another chronic autoimmune disease linked to anti-centromere. About 9.1% of patients with this liver disease have the antibody in their blood. If you have both scleroderma and primary biliary cirrhosis, the rate rises to 50%. The presence of anti-centromere in your blood may mean a higher risk of cirrhosis and portal hypertension. Some studies show that patients with the antibody may have more severe symptoms and need closer monitoring and treatment.
Other Autoimmune Disorders
You may see anti-centromere in other connective tissue diseases, but less often. These include rheumatoid arthritis and lupus. The antibody helps doctors find the right diagnosis and guide your treatment. Anti-centromere is a key marker for scleroderma, crest syndrome, and other autoimmune diseases. If you have symptoms like blood changes, skin thickening, or raynaud’s phenomenon, your doctor may check for this antibody in your blood. Early detection helps you get the best treatment and manage your symptoms.
Test Process
Preparation
You do not need to do anything special before your anti centromere antibody test. Most people can eat and drink as usual. Your doctor may ask about any medicines you take. Some drugs can affect your test results, so always share this information. You should also know that certain problems, like improper sample handling or choosing the wrong test, can change your results.
- No special preparation needed
- Tell your doctor about all medications
- Make sure the sample is collected and handled correctly
Tip: Always let your healthcare provider know about any health conditions or supplements you use.
Procedure
Your healthcare provider will collect a blood sample for the anti-centromere test. The process is quick and simple. A nurse or technician will draw blood from your arm, usually using a small needle. The blood goes into a special tube for testing.
| Specimen Type | Temperature | Time |
|---|---|---|
| Serum | Refrigerated | 21 days |
| Serum | Frozen | 21 days |
- Preferred specimen: Serum gel
- Acceptable specimen: Red top tube
- Use a plastic vial for submission
- Needed volume: 0.5 mL (minimum 0.35 mL)
- Centrifuge and move serum into the vial
Your sample will be sent to a lab. The lab keeps the serum cold or frozen to protect it. This helps make sure your results are accurate.
After the Test
You can return to your normal activities after the blood draw. Most people feel fine, but you might have a small bruise. Your results usually come back in 14 to 21 days. Sometimes, extra tests may take longer.
- Results take about 2 to 3 weeks
- Your doctor will explain what the results mean
| ACA Test Results | Doctor to Visit | Reason to See Doctor |
|---|---|---|
| Positive | Rheumatologist | Evaluate for systemic sclerosis |
| Negative | Primary Care | Routine follow-up or other concerns |
If your anti-centromere test is positive, your doctor may send you to a rheumatologist. This specialist checks for diseases like systemic sclerosis. If your test is negative, your primary care doctor will help you decide on next steps.
Test Results
Positive Result
When you receive a positive anti centromere antibody test result, your doctor will look closely at your symptoms. A positive result has a high positive predictive value for limited cutaneous systemic sclerosis and CREST syndrome. If you have a positive test, you may notice symptoms like Raynaud’s phenomenon, sclerodactyly, or skin changes. In Sjögren’s syndrome, a positive test often means you have a higher chance of Raynaud’s phenomenon and trouble swallowing, but you may have fewer problems with dry eyes or other autoantibodies. Most people with a positive anti-centromere test do not develop full systemic sclerosis. Instead, you may show symptoms that fall between those with a negative test and those with systemic sclerosis. The positive predictive value of this test is highest when you already have symptoms that match these diseases.
A positive result does not always mean you will develop a serious disease. Your doctor will use your test result, symptoms, and other findings to decide what comes next.
Negative Result
A negative anti-centromere test result means the antibody was not found in your blood. This result has a high negative predictive value for limited cutaneous systemic sclerosis and CREST syndrome. If you have a negative test, you are less likely to have these diseases. The negative predictive value is strongest when you do not have symptoms like Raynaud’s phenomenon or skin thickening. However, a negative result does not rule out all autoimmune diseases. Your doctor may look for other causes if you still have symptoms. Sometimes, people with early or mild disease may still have a negative test.
Next Steps
If your anti-centromere test is positive, your doctor may order more tests to check for organ involvement or other problems. These steps help your doctor understand your health better and plan your care. You may need:
- Imaging studies to look at your organs
- Esophageal manometry to check your swallowing
- Skin biopsies for more information
- Pulmonary function tests to see how your lungs work
If your test is negative, your doctor may suggest regular check-ups or other tests based on your symptoms. You should always talk with your healthcare provider about your results and what they mean for you. The positive predictive value and negative predictive value of the anti-centromere test help your doctor decide how to guide your care.
Limitations and Risks
False Positives and Negatives
You may wonder if the anti centromere antibody test can give you a wrong result. False positives are very rare with this test. Almost no one gets a false positive result when testing for centromere antibodies. This means that if your test shows you have the antibody, it is very likely correct. False negatives can happen, but they are not common. Sometimes, people with early or mild disease may not show the antibody in their blood. Your doctor looks at your symptoms and other test results to make sure you get the right diagnosis.
- False positives are extremely rare.
- False negatives may occur in early or mild disease.
- Your doctor uses other information to confirm your diagnosis.
If you have questions about your test result, ask your doctor to explain what it means for you.
Safety
You may feel nervous about getting the anti-centromere test. The procedure is safe for most people. The test uses a standard blood draw, which carries very little risk. You might feel mild discomfort when the needle goes in. Some people get a small bruise or redness at the spot. Rarely, you could get an infection where the blood was drawn. Most people do not have any problems after the test.
- The test is safe and uses a simple blood draw.
- Mild discomfort or bruising may happen.
- Infection at the blood draw site is very rare.
Tip: If you notice swelling or pain after your blood draw, let your healthcare provider know.
You play an important role in your own health. The anti centromere antibody helps you and your healthcare providers find autoimmune diseases early. Early detection with the anti-centromere test can improve patient care and guide your next steps. You should talk with healthcare providers about your results. Healthcare providers can explain what your test means. Healthcare providers may suggest more tests or regular check-ups. Healthcare providers help you understand your risk. Healthcare providers support you in managing symptoms. Healthcare providers can answer your questions. Healthcare providers work with you for the best outcome. The table below shows how early detection with healthcare providers can impact your future:
| Finding | Description |
|---|---|
| ACA Presence | Associated with 80% likelihood of developing autoimmune diseases, particularly limited cutaneous systemic sclerosis (lcSSc). |
| Low Titers of ACA | Linked to decreased frequency of autoimmune diseases, indicating a potential influence on disease prognosis. |
Stay aware and keep in touch with healthcare providers for ongoing monitoring and better health.
FAQ
What does a positive anti-centromere antibody test mean?
A positive result means you have antibodies that target the centromere in your cells. This often points to limited cutaneous systemic sclerosis or CREST syndrome. Your doctor will use this result with your symptoms to guide your care.
Can you have anti-centromere antibodies without having an autoimmune disease?
Yes, some healthy people may have low levels of these antibodies. However, high levels usually suggest an autoimmune condition. Your doctor will look at your symptoms and other test results to decide what it means for you.
How often should you repeat the anti-centromere antibody test?
Doctors usually do not repeat this test often. If your symptoms change or new symptoms appear, your doctor may order another test. Most people only need the test once for diagnosis.
Are there ways to lower anti-centromere antibody levels?
No proven treatments lower these antibody levels directly. Doctors focus on treating your symptoms and managing the underlying autoimmune disease. Healthy habits and regular check-ups help you stay well.
What should you do if your test is positive but you feel healthy?
You should talk with your doctor. A positive test does not always mean you will get sick. Your doctor may suggest regular check-ups to watch for any new symptoms.