Antibody knowledge
Comparing Strep Test Kits and ELISA Immunoassays for Streptococcal Diagnosis

Accurate and fast diagnosis helps you prevent serious complications from streptococcal pharyngitis. Health professionals often choose a strep test kit because it gives results quickly and helps guide treatment. You see both strep test kits and ELISA immunoassays in clinics and labs today. Each method shows unique strengths and some limits.
Over 500,000 deaths happen worldwide each year from Streptococcus pyogenes.
Timely diagnosis reduces transmission and keeps mild cases from spreading after 24 hours of antibiotics.
Key Takeaways
Strep test kits provide rapid results, allowing for immediate treatment decisions in clinics. This helps prevent the spread of infection.
ELISA immunoassays offer higher sensitivity and specificity, making them ideal for detailed analysis in laboratory settings.
Choose the diagnostic method based on your setting: use strep test kits for quick answers and ELISA for confirmation or outbreak tracking.
Consider patient needs and risk factors when selecting a test. High-risk groups may require more reliable diagnostic methods.
Using accurate tests improves patient outcomes by ensuring timely treatment and reducing unnecessary antibiotic prescriptions.
Diagnosis: Strep Test Kits vs. ELISA
Clinical Preference
When you need to diagnose strep throat quickly, most clinics choose strep test kits. These kits give you results in minutes. Doctors often use them during your visit. You can start treatment right away if the test is positive. ELISA immunoassays, on the other hand, usually take longer. You often find them in hospital labs or research settings. ELISA tests can detect smaller amounts of strep antigens, but you may wait hours or even a day for results.
You want to know which test works best. Sensitivity tells you how well a test finds people with strep. Specificity shows how well it avoids false positives. Here is a table that shows how different tests compare:
Test Kit | Sensitivity | Specificity |
|---|---|---|
Abbott TestPack Strep A | 79% | 98% |
Direct Strep A EIA (Roche) | 79% | 63% |
Respirastick | 55% | 96% |
Reveal Colour Strep A | 82% | 83% |
Tandem ICON Strep A | 78% | 98% |
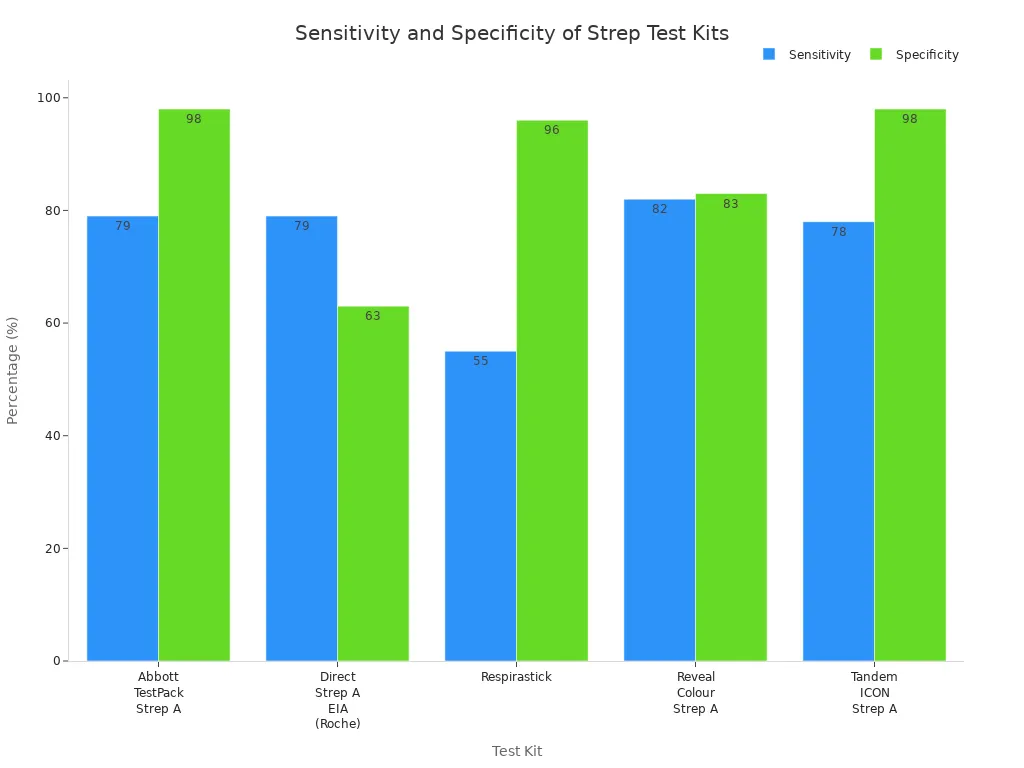
You see that most strep test kits have high specificity. This means you rarely get a false positive. Sensitivity varies more. Some tests miss more cases than others. ELISA immunoassays, like the Direct Strep A EIA, show similar sensitivity to rapid kits but lower specificity in some studies. You should remember that no test is perfect. Doctors sometimes follow up a negative rapid test with a throat culture, which is the gold standard.
Situational Use
You may wonder when to use each test. If you work in a busy clinic or emergency room, you need fast answers. Strep test kits fit this need. You can test a patient and decide on antibiotics in one visit. This helps stop the spread of infection and improves patient care.
ELISA immunoassays work better in settings where speed is less important. You might use them in a hospital lab or for research. ELISA can help when you need to confirm a diagnosis or when you want to track outbreaks. Some clinics use ELISA if they need to test many samples at once.
Tip: Always consider the setting and the needs of your patients. Fast tests help in clinics. More detailed tests help in labs.
You should use this comparison to guide your choice. Think about how quickly you need results, how accurate you want the test to be, and what resources you have.
Strep Test Kits: Rapid Testing

How Strep Test Kits Work
You use a strep test kit to check for group A streptococcus in your throat. Most clinics rely on a rapid antigen detection test for this purpose. The rapid antigen detection tests work by finding specific proteins from the bacteria. You collect a throat swab and place it in the strep test kit. The kit uses a rapid method to show results in minutes.
Here is a table that shows how different rapid antigen detection test types work:
Test Type | Mechanism of Action |
|---|---|
Latex Fixation Test | Uses latex beads coated with antigens that agglutinate around GAS antibodies if present. |
Lateral Flow Test | Sample applied to nitrocellulose film; if GAS antigens are present, they migrate to form a visible line. |
Optical Immunoassay | Mixes sample with labeled antibodies and substrate; color change indicates presence of GAS antigen. |
You see that each strep test kit uses a rapid process to detect the bacteria. The rapid antigen detection test gives you answers quickly, which helps you decide on treatment during your visit.
Types of Strep Test Kits
You find several types of strep test kit in clinics and hospitals. The most common are rapid antigen detection tests. These include lateral flow tests, latex fixation tests, and optical immunoassays. Each rapid antigen detection test has a unique way to show results, but all aim for speed and accuracy.
Lateral flow rapid antigen detection tests show a colored line if strep is present.
Latex fixation rapid antigen detection tests use beads that clump together.
Optical immunoassay rapid antigen detection tests change color when they detect strep.
The average sensitivity for rapid antigen detection tests is about 86%. Specificity reaches 95%. Some studies report sensitivity as low as 58% or as high as 96%, with specificity ranging from 63% to 100%. You can trust a strep test kit to give you a rapid answer, but doctors may confirm negative results with a throat culture.
Use in Point-of-Care
You use a strep test kit most often in point-of-care settings. The rapid antigen detection test helps you get results during your appointment. This rapid process means you do not wait for lab results. You can start antibiotics right away if needed.
Point-of-care rapid antigen detection tests save time and money. They cost less than traditional lab tests and help you avoid unnecessary antibiotics for viral infections. You improve patient care and help stop the spread of strep. Rapid streptococcal antigen detection tests make point-of-care diagnosis possible in clinics, schools, and even pharmacies.
Tip: You should use a strep test kit in point-of-care settings when you need a rapid answer. This helps you treat patients quickly and prevent complications.
ELISA Immunoassays: Laboratory Diagnosis

ELISA Process
You use ELISA immunoassays in a laboratory to detect streptococcal infections. ELISA stands for Enzyme-Linked Immunosorbent Assay. This test helps you find specific antigens or antibodies in a sample. You start by adding your sample to a plate coated with antibodies. If the target antigen is present, it binds to the antibody. You then add an enzyme-linked antibody that attaches to the antigen. When you add a special substrate, the enzyme causes a color change. You measure this color to see if the sample contains streptococcal markers.
ELISA tests give you a clear result based on color intensity. You can use this method to confirm a diagnosis or track the spread of infection.
ELISA Types
You find several types of ELISA immunoassays for streptococcal diagnosis. The most common are direct, indirect, and sandwich ELISA. Each type uses a different method to detect antigens or antibodies. Indirect ELISA helps you find antibodies against Streptococcus in blood samples. Sandwich ELISA detects antigens directly from throat swabs.
Researchers have developed advanced ELISA methods, such as the GMD-ELISA. This test uses recombinant GMD protein instead of whole bacterial antigens. You get better sensitivity and specificity with GMD-ELISA. It does not cross-react with other streptococcal species. This makes your results more reliable and accurate.
ELISA Type | Target Detected | Sample Used | Sensitivity | Specificity |
|---|---|---|---|---|
Indirect ELISA | Antibodies | Blood serum | High | High |
Sandwich ELISA | Antigens | Throat swab | High | High |
GMD-ELISA | Antibodies | Blood serum | Very High | Very High |
Lab Requirements
You need special equipment and trained staff to run ELISA immunoassays. You work in a laboratory with microplate readers, pipettes, and reagents. ELISA tests take longer than rapid strep kits. You may wait several hours or a full day for results. You get high sensitivity and specificity, but you need more resources and time.
Tip: Use ELISA immunoassays when you need detailed and accurate results, especially for research or outbreak investigations.
Test Comparison: Accuracy and Speed
Sensitivity and Specificity
You want to choose the best diagnostic methods for detecting group a beta-haemolytic streptococci. Strep a rapid test device uses antigen detection to find the bacteria quickly. Most strep a rapid test devices show high sensitivity and specificity, but some miss cases. ELISA immunoassays also use antigen detection, but they work in a lab and can find smaller amounts of bacteria. You see high sensitivity and specificity in ELISA tests, especially with advanced types like GMD-ELISA.
Throat culture stands as the gold standard for diagnostic accuracy. You use it to confirm cases when rapid tests or ELISA results are unclear. Throat cultures detect group a beta-haemolytic streptococci with very high sensitivity and specificity, but you wait longer for results.
Diagnostic Method | Sensitivity | Specificity | Diagnostic Accuracy |
|---|---|---|---|
Strep A Rapid Test Device | 58-96% | 63-100% | Good |
ELISA Immunoassays | High | High | Very Good |
Throat Culture | >95% | >95% | Excellent |
Note: You should use throat culture when you need the highest diagnostic accuracy, but strep a rapid test device and ELISA immunoassays offer strong diagnostic utility for most cases.
Turnaround Time
You need fast results to treat group a beta-haemolytic streptococci and prevent complications. Strep a rapid test device gives you results in 10-15 minutes. You use antigen detection at the point of care, so you do not wait for lab processing. ELISA immunoassays take longer because you need lab equipment and trained staff. You may wait several hours or a full day for ELISA results. Throat cultures require even more time. You often wait 24-48 hours for a final answer.
Here is a table that shows average turnaround times:
Test Type | Average Turnaround Time |
|---|---|
Strep Test Kits | 10-15 minutes |
ELISA Immunoassays | Several hours to 1 day |
Throat Cultures | 24-48 hours |
You see that strep a rapid test device offers the fastest results. ELISA immunoassays and throat cultures take longer, but they provide high diagnostic accuracy.
Cost and Resources
You want to use diagnostic methods that fit your clinic’s budget and resources. Strep a rapid test device costs less than ELISA immunoassays or throat cultures. You use antigen detection with simple kits, so you do not need special equipment. ELISA immunoassays require lab tools, reagents, and trained staff. You spend more money and time to run these tests. Throat cultures also need lab space and skilled workers, but they give you the highest diagnostic accuracy.
Strep a rapid test device: Low cost, easy to use, fast antigen detection.
ELISA immunoassays: Higher cost, need lab equipment, detailed antigen detection.
Throat cultures: Moderate cost, need lab staff, highest diagnostic accuracy.
Tip: You should use strep a rapid test device for quick screening and ELISA immunoassays or throat cultures when you need confirmation or detailed results.
You improve patient care when you match the diagnostic utility of each method to your clinic’s needs. You stop the spread of group a beta-haemolytic streptococci by choosing the right test for each situation.
Clinical Application: Guidelines for Diagnosis
Point-of-Care vs. Lab Settings
You face different choices for diagnosing group a streptococcus depending on your setting. In clinics, point-of-care testing helps you manage infection quickly. You get results fast and can start treatment during the same visit. In labs, you use more advanced diagnostic methods like ELISA immunoassays. These tests take longer but give you detailed results. New nucleic acid technologies now offer sensitive and specific diagnostic options for outpatient care. You must balance speed, accuracy, and cost when choosing a test.
Point-of-care tests give rapid answers for group a streptococcus.
Laboratory tests provide higher sensitivity and specificity for infection.
Rapid nucleic acid tests now bring lab-level diagnostic accuracy to clinics.
You should consider the quality and reliability of each diagnostic method before making a decision.
Evidence-Based Recommendations
You want to follow the best guidelines for diagnosing group a streptococcus. Experts recommend using rapid antigen detection tests for quick screening. If you need more accurate results, you can use ELISA immunoassays or throat cultures. Rapid nucleic acid tests now show even higher sensitivity and specificity. Studies show these tests reach 97.5% sensitivity and 95.1% specificity for group a streptococcus. You can use rapid nucleic acid tests as stand-alone diagnostic tools for infection. These tests help you avoid missed cases and reduce unnecessary antibiotics.
Special Populations
You must pay special attention to certain groups when diagnosing group a streptococcus infection. Children, older adults, and people with weakened immune systems may need more reliable diagnostic methods. In these cases, you should use tests with high sensitivity to avoid missing infection. Rapid nucleic acid tests and ELISA immunoassays work well for these populations. You help prevent complications and improve outcomes by choosing the right diagnostic approach.
Tip: Always match your diagnostic method to your patient’s needs and your clinical setting.
Practical Implications for Providers
Decision-Making
You face many choices when diagnosing streptococcal pharyngitis. You want to pick the test that fits your clinic, your resources, and your patients. Rapid strep test kits work best when you need answers fast. You can use them in busy clinics, schools, or urgent care centers. These kits help you decide on treatment during the same visit. ELISA immunoassays give you more detailed results, but you need a lab and trained staff. You may use ELISA when you want to confirm a diagnosis or track an outbreak.
You should ask yourself these questions before choosing a test:
Do you need results right away?
Is your patient at high risk for complications?
Can you access a laboratory?
How many samples do you need to test?
Tip: Use rapid strep test kits for quick decisions. Choose ELISA immunoassays for detailed analysis or when you need to test many samples.
Patient Outcomes
Your choice of diagnostic method affects your patients. If you use a highly sensitive rapid test, such as the Strep A OIA, you can start treatment immediately. This approach helps you prevent complications from untreated infections. You also avoid giving antibiotics when they are not needed. Reliable tests improve patient outcomes by making sure only those with true infections get medicine.
You cannot rely on symptoms alone to diagnose strep throat. Studies show that clinical signs do not always match test results. You need a reliable test to guide your decisions. When you use accurate diagnostic tools, you protect your patients from unnecessary drugs and help them recover faster.
Immediate testing leads to faster treatment.
Fewer unnecessary antibiotics mean less resistance.
Reliable diagnosis lowers the risk of missed infections.
Note: You improve patient care when you match your diagnostic method to your clinical setting and your patient’s needs.
You should use rapid strep test kits for quick answers when you suspect streptococcal pharyngitis. ELISA immunoassays work best in labs where you need high accuracy or must confirm results. Clinical guidelines remind you to match your test choice to the urgency and setting.
Sensitivity | Specificity | Antibiotic Use Impact | |
|---|---|---|---|
RADT | Moderate | Moderate | More unnecessary prescriptions |
NAAT | High | High | Reduces unnecessary use |
New trends include rapid molecular tests and AI tools that help you improve diagnosis of streptococcal pharyngitis and reduce unnecessary antibiotics.
FAQ
What is the main difference between a strep point-of-care test and ELISA for streptococcal diagnosis?
You use a strep point-of-care test for quick diagnosis in clinics. ELISA gives you more detailed results in labs. Both methods help with detection of streptococcal infections, but ELISA offers higher sensitivity and specificity.
How does sensitivity affect streptococcal diagnosis?
Sensitivity shows how well your test finds true cases of streptococcal infection. High sensitivity means you miss fewer cases. You improve diagnosis by choosing tests with strong sensitivity, especially for early detection.
Why is specificity important in streptococcal detection?
Specificity tells you how well your test avoids false positives. High specificity means you only diagnose true streptococcal infections. You reduce unnecessary treatment by using tests with high specificity.
Can you use a point-of-care test for all streptococcal diagnosis situations?
You use a point-of-care test for rapid diagnosis in clinics. For complex cases or outbreaks, you need ELISA or throat cultures. These methods offer higher sensitivity and specificity for streptococcal detection.
What should you do if your rapid test for streptococcal diagnosis is negative?
You should confirm negative results with a throat culture or ELISA. These tests have higher sensitivity and specificity. You avoid missed diagnosis and ensure accurate detection of streptococcal infections.

