News & Events
Anti-Ro Antibody Explained for Patients and Clinicians
You might wonder what the anti ro antibody is and why it matters. This antibody, also known as anti-ro/ssa antibodies, plays a key role in autoimmunity. Doctors look for anti-ro antibody when diagnosing diseases like Sjögren’s syndrome or lupus. In the general population, only 0.5–2.7% have anti-ro antibodies, but in autoimmune diseases, the rate can reach up to 100%.
| Population Group | Prevalence of Anti-Ro Antibodies |
|———————————-|———————————-|
| General Population | 0.5–2.7% |
| Patients with Autoimmune Diseases | 15%–100% (varies by subgroup) |
Understanding your test results helps you and your doctor manage symptoms and risks early.
Key Takeaways
- Anti-Ro antibodies are crucial in diagnosing autoimmune diseases like Sjögren’s syndrome and lupus. Understanding your test results helps manage symptoms early.
- There are two main types of anti-Ro antibodies: Ro52 and Ro60. Each type is linked to different health risks and symptoms, guiding treatment decisions.
- A positive anti-Ro antibody test indicates a higher risk for autoimmune diseases. Regular checkups and monitoring are essential for managing your health.
- If you have anti-Ro antibodies and plan to get pregnant, consult your doctor for special monitoring to protect both you and your baby.
- Lifestyle changes, such as sun protection, a balanced diet, and regular exercise, can help manage symptoms and improve overall health.
What Is Anti-Ro Antibody?
Definition and Role
You may hear your doctor mention the anti ro antibody when discussing autoimmunity. This antibody, also called anti-ro/ssa antibodies, targets specific proteins inside your cells. Your immune system usually protects you from germs. Sometimes, it mistakenly attacks your own tissues. This process is called autoimmunity.
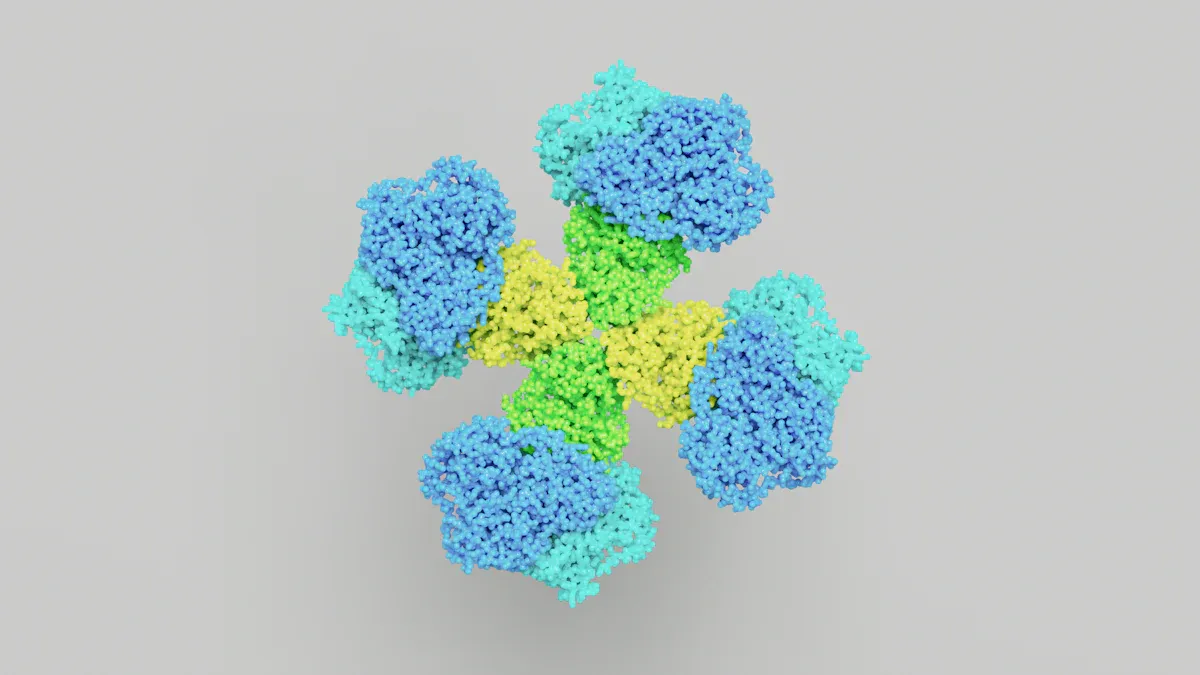
Anti-ro antibody attaches to proteins named Ro52 and Ro60. These proteins help your cells work properly. Ro60 helps make 5S rRNA, which is important for building proteins in your body. Ro52 sits mostly in the cytoplasm, but its exact job is less clear. When your immune system creates anti-ro antibodies, it can cause inflammation and tissue damage, especially if your cells are under stress.
Note: Anti-ro/ssa antibodies can show up in people with autoimmune diseases like Sjögren’s syndrome or lupus. Sometimes, healthy people may also have these antibodies, but this is rare.
Here is a table that shows the molecular structure and function of these proteins:
| Aspect | Details |
|---|---|
| Ro Proteins | Ro60 and Ro52 |
| Molecular Structure | Ro60 is a 60 kDa protein, and Ro52 is a 52 kDa protein. |
| Gene Location | Ro60 gene is on chromosome 19, Ro52 gene is on chromosome 11. |
| Function of Ro60 | Important for maintaining production of functional 5S rRNA, often complexed with La protein. |
| Function of Ro52 | Mainly located in the cytoplasm; its function is less defined compared to Ro60. |
| Clinical Associations | Anti-Ro52 and anti-Ro60 antibodies have different clinical associations. |
| Interaction | Initial suggestions of interaction between Ro52 and Ro60 were not confirmed in later studies. |
Types: Ro52 and Ro60
You will often hear about two main types of anti-ro antibodies: Ro52 and Ro60. Both belong to the same family, but they have different roles and clinical meanings.
- Ro60 is mostly found in the nucleus of your cells. It is crucial for making 5S rRNA, which helps your cells build proteins.
- Ro52 is mainly in the cytoplasm. Scientists are still learning about its exact function, but they know it plays a part in the immune response.
Doctors test for both types because they can point to different health problems. For example:
- If you have both Ro52 and Ro60 antibodies, you may have a higher chance of symptoms like dry mouth and dry eyes (xerostomia and xerophthalmia).
- If you have only Ro52 antibodies, you may face a higher risk of muscle inflammation (myositis) or certain cancers.
- If you have only Ro60 antibodies, you may be more likely to develop systemic lupus.
Here is a table that shows how different combinations of these antibodies relate to clinical features:
| Antibody Group | Clinical Association | Statistical Significance |
|---|---|---|
| Ro52+Ro60+ | Hypergammaglobulinemia | p = 0.002 |
| Ro52+Ro60- | Anemia | p = 0.03 |
| Ro52+Ro60- | Renal Insufficiency | p = 0.01 |
| Ro52-Ro60+ | Diffuse skin involvement in systemic sclerosis | N/A |
| Isolated Ro60 Ab | More frequent diagnosis of systemic lupus | N/A |
| Isolated Ro52 Ab | Associated with inflammatory myositis and rheumatism | N/A |
You can see that the presence of these antibodies can help your doctor predict which symptoms or risks you might face. The chart below shows how different combinations of anti-Ro and anti-La antibodies relate to specific symptoms in autoimmune diseases:
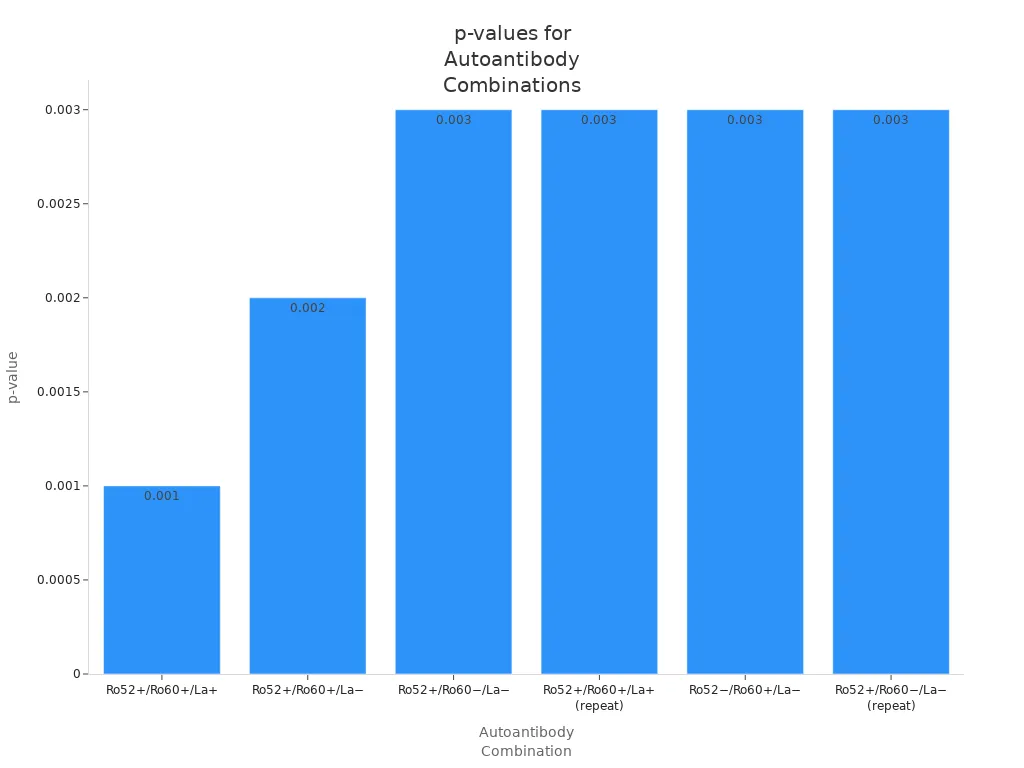
Tip: Laboratories and doctors need to check for both Ro52 and Ro60. Each type gives important clues about your health and helps guide your treatment.
Recent research shows that anti-Ro52 antibodies can help doctors predict how connective tissue diseases might progress. For example, people with anti-Ro52 antibodies may have a higher risk of lung problems. This information helps your doctor plan the best care for you.
Anti-Ro Antibodies and Autoimmune Diseases
You may wonder how anti-ro antibodies connect to different autoimmune diseases. These autoantibodies play a key role in several conditions. Doctors use them as a marker to help diagnose and predict disease activity. The presence of these antibodies can affect your symptoms, treatment, and even the risks for your family.
Sjögren’s Syndrome
Sjögren’s syndrome is one of the most common diseases linked to anti-ro/ssa antibodies. You may see these antibodies in both primary and secondary forms of the disease. They are much more common in patients with sjögren’s syndrome than in healthy people.
- About 53.2% of patients with primary sjögren’s syndrome test positive for anti-ro/ssa antibodies.
- If you have these antibodies, you may get diagnosed at a younger age.
- You might feel more tired and have more severe symptoms.
- Systemic problems, such as swollen glands, skin rashes, lung issues, and blood changes, are more likely.
- Joint pain and swelling can happen more often.
- Doctors may need to use stronger treatments, like immunosuppressants or steroids, if you have these antibodies.
You can see that anti-ro antibodies and autoimmune diseases often go together. The clinical manifestations related to anti-ro antibodies in sjögren’s syndrome can help your doctor decide on the best care plan.
Note: Anti-ro antibodies are much less common in healthy people, but they do appear sometimes. This means a positive test does not always mean you have an autoimmune disease.
Systemic Lupus Erythematosus
Systemic lupus erythematosus, or SLE, is another disease where anti-ro antibodies are important. You may hear your doctor talk about SLE if you have symptoms like joint pain, skin rashes, or kidney problems.
- Between 25% and 50% of people with SLE have anti-ro antibodies.
- If you test positive, you may have a more active disease.
- Doctors often use more glucocorticoids and immunosuppressants for patients with these antibodies.
- You may notice symptoms like protein in your urine or dry mouth and eyes.
The presence of anti-ro antibody in SLE can signal a higher risk for organ involvement. Your doctor may monitor you more closely and adjust your treatment if you have these autoantibodies. Anti-ro antibodies can serve as a marker for disease activity and help guide your care.
Neonatal Lupus
If you are pregnant and have anti-ro antibodies, your baby may be at risk for neonatal lupus. This condition happens when these antibodies cross the placenta and affect the baby.
| Clinical Manifestation | Description | Resolution Timeline |
|---|---|---|
| Congenital Heart Block (CHB) | Permanent heart rhythm problem in a normal heart. | Permanent |
| Cutaneous Lupus | Skin rash, often appears in the second or third month. | Usually resolves by 9 months |
| Hepatobiliary Disease | Liver problems, such as cholestasis or increased liver enzymes. | 10%–25% of cases, resolves by 9 months |
| Hematological Manifestations | Blood problems like anemia or low white cells. | Usually resolves by 9 months |
| CNS Involvement | Rare brain or nerve problems. | N/A |
Most symptoms, except for heart block, go away by 9 months. Your doctor will watch your baby closely if you have anti-ro antibodies during pregnancy.
Other Associations
Anti-ro antibodies can show up in other diseases, not just sjögren’s syndrome or lupus. You may see them in muscle diseases, lung problems, or other autoimmune conditions.
| Group | Conditions Associated | Frequency |
|---|---|---|
| Ro52 + Ro60- | Inflammatory Myositis, Inflammatory Rheumatism | Higher prevalence |
| Ro52 + Ro60+ | Primary Sjögren Syndrome | Most likely diagnosis |
| Ro52-Ro60+ | Systemic Lupus | Most frequent diagnosis (48.5%) |
| Condition | Clinical Significance |
|---|---|
| Autoimmune Diseases | High prevalence (73%) in some groups; anti-Ro52 not always linked to disease. |
| Pulmonary Infections | Testing for anti-Ro52 may help diagnose lung diseases. |
| Antisynthetase Syndrome | Anti-Ro52 can help diagnose this rare muscle and lung disease. |
| Autoimmune Idiopathic Interstitial Lung Disease | Doctors use anti-Ro52 to help classify and diagnose these lung problems. |
You can see that the anti ro antibody is not only a marker for classic autoimmune diseases. It can also help doctors find and treat other rare or complex conditions. The presence of this autoantibody gives important clues about your health and helps guide your care.
Clinical Significance of Anti-Ro Antibody
Diagnosis and Prognosis
When your doctor orders an anti-ro antibody test, they look for important clues about your health. This test helps with diagnosis and classification of autoimmune diseases. If you have a high level of anti-ro antibodies (for example, a titer greater than 1:640), you are more likely to have an autoimmune disorder. The anti-ro antibody acts as a marker for diseases like systemic lupus erythematosus, mixed connective tissue disease, Sjögren’s syndrome, or scleroderma. If you test positive but do not have a diagnosis yet, your doctor may want to monitor you over time. This helps catch any signs of autoimmunity early.
Here is a table that shows how anti-ro/ssa antibodies help in diagnosis and prognosis:
| Evidence Type | Description |
|---|---|
| Antibody Titer | High concentrations of anti-Ro antibodies (titer >1:640) suggest the presence of an autoimmune disorder. |
| Diagnostic Implications | Presence of anti-Ro antibodies increases the likelihood of conditions such as SLE, MCTD, Sjögren’s, or scleroderma. |
| Monitoring | If no diagnosis is made initially, patients should be monitored for the development of ANA-associated diseases. |
You can see that anti-ro antibodies play a key role in diagnosis and predicting how a disease might progress. This clinical importance helps guide your care and treatment.
Symptoms and Risks
If you have anti-ro/ssa antibodies, you may notice certain symptoms. These autoantibodies are linked to photosensitivity, which means your skin reacts strongly to sunlight. In childhood-onset SLE, about 73% of patients with these antibodies have photosensitivity, compared to 65% without them. You might also see mild skin problems, like rashes.
Anti-ro antibodies can affect more than just your skin. You may face inflammation in different organs. Some people with anti-ro52 antibody have more severe problems, such as lung disease or even cancer. The presence of this autoantibody can lower survival rates in some patients.
Here are some risks linked to anti-ro antibodies:
- Higher chance of photosensitivity and skin symptoms
- Increased risk of inflammation in organs like the lungs
- Possible link to cancer in certain cases
- Lower survival rates for some patients with persistent positivity
Doctors use the presence of anti-ro antibodies as a marker to watch for these risks. This helps you and your healthcare team manage your health more closely.
Testing for Anti-Ro Antibody

Test Methods
Doctors use several laboratory methods to detect the anti ro antibody. Each method has different strengths. The most common tests include ELISA, immunoblotting, and immunofluorescence. ELISA is popular because it is quick and sensitive. Immunoblotting helps confirm results. Immunofluorescence can show the presence of autoantibodies in your blood by making them glow under a special microscope. Some labs use RNA precipitation assays, which have the highest sensitivity and specificity.
| Method | Sensitivity (%) | Specificity (%) |
|---|---|---|
| RNA Precipitation Assay | Highest | Highest |
| ELISA (anti-Ro/SS-A) | 96 | N/A |
| Immunoblotting (anti-Ro/SS-A) | 80 | N/A |
| Counterimmunoelectrophoresis | Comparable | N/A |
Before testing, you should tell your doctor about any medicines or supplements you take. Sometimes, you may need to fast for a few hours. Drinking water helps make the blood draw easier.
Interpreting Results
When you get your results, your doctor will look at the levels of autoantibody and your symptoms. A positive test means your body has made autoantibodies against Ro proteins. This marker often appears in autoimmune diseases. For example, about 60-70% of people with Sjögren syndrome and 25% with lupus have a positive test. Age can also play a role. Both younger and older people may show positive results.
| Condition | Percentage of Cases |
|---|---|
| Sjögren syndrome | 60-70% |
| Systemic lupus erythematosus (SLE) | 25% |
| Age older than 50 years | Associated |
| Age younger than 22 years | Associated |
Note: Sometimes, healthy people can have a positive test. Your doctor will use other signs and symptoms to decide if you have an autoimmune disease.
Limitations
No test is perfect. Some testing methods, like ELISA, can give false positives. This means the test says you have the antibody when you do not. Other methods, like the Ouchterlony assay, may miss the antibody and give a false negative. These errors can lead to wrong diagnoses or missed treatment. If you get a false positive, you might worry or get unnecessary medicine. If you get a false negative, your doctor might miss signs of autoimmunity. Always talk with your doctor about your results and what they mean for your health.
Maternal and Fetal Implications
Pregnancy Risks
If you have anti ro antibody during pregnancy, you face special risks. Your immune system may attack your own tissues, a process called autoimmunity. This can affect both you and your baby. Doctors see higher rates of pregnancy complications in women with these antibodies.
You may experience:
- More miscarriages. Studies show about 20% of pregnancies end in miscarriage.
- Increased risk of intrauterine fetal demise (IUFD), which happens in about 5% of cases.
- Higher chance of preterm birth. About 17% of live births arrive early.
- Babies born with low birth weight, especially if you have systemic lupus erythematosus.
- Possible placental problems, which can lead to mid-pregnancy miscarriages.
Doctors recommend close monitoring if you test positive for anti ro antibody. You should talk with your healthcare team about your risks and the best plan for your pregnancy.
Neonatal Outcomes
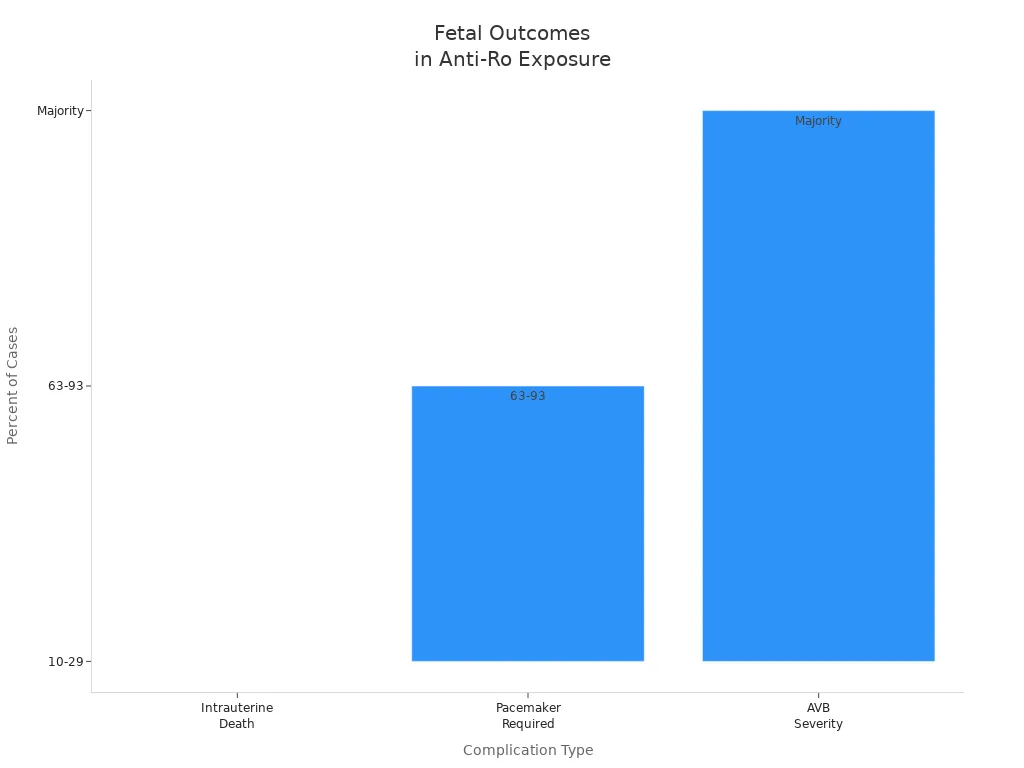
Your baby may face health challenges if exposed to anti ro antibody during pregnancy. The most serious risk is congenital heart block (CHB). This condition affects the heart’s rhythm and can be life-threatening.
| Finding | Description |
|---|---|
| Risk of CHB | Babies exposed to maternal anti-Ro/SSA and anti-La/SSB antibodies have a higher risk. |
| Prognosis | Many babies need a pacemaker. Some face poor outcomes or intrauterine death. |
| Intrauterine Death | 10% to 29% of affected fetuses do not survive pregnancy. |
| Pacemaker Requirement | 63% to 93% of babies with CHB need a permanent pacemaker. |
| AVB Severity | Most cases show complete heart block at diagnosis. |
| Antibody Levels | Higher antibody levels mean greater risk for heart problems and tissue damage. |
Doctors use several strategies to protect your baby. You may get weekly or biweekly fetal echocardiograms to check your baby’s heart. Some mothers monitor fetal heart rate at home three times a day. If your antibody levels are low, your baby’s risk for heart block drops. No cases of fetal heart block have been seen in mothers with low antibody titers.
| Monitoring Strategy | Description | Outcome |
|---|---|---|
| Weekly/Biweekly Fetal Echocardiograms | Standard care for anti-Ro positive pregnancies | May miss rapid progression of AV block |
| Home Monitoring of Fetal Heart Rhythm | Check fetal heart rate three times daily | Detected all abnormal rhythms in high-titer cases |
| Risk Stratification by Antibody Titer | Low titers (<1000 units/mL) mean low risk | No cases of fetal AV block in low-titer group |
You should discuss these options with your doctor early in pregnancy. Personalized monitoring helps lower risks for you and your baby.
What to Do After a Positive Test
For Patients
Getting a positive anti ro antibody test can feel overwhelming. You may wonder what steps to take next. Here are some practical actions you can follow:
- Talk with your doctor about what your results mean for your health. Ask questions if you do not understand something.
- Protect your skin from sunlight. Wear hats, use sunscreen, and avoid being outside during peak sun hours. Sun exposure can trigger flare-ups in autoimmunity.
- Eat a balanced diet. If you have high cholesterol, choose low-fat foods. Your doctor may suggest vitamin D supplements, especially if you avoid the sun.
- Exercise regularly. Staying active helps prevent muscle loss, bone weakness, and fatigue.
- Do not smoke. Smoking can make symptoms worse and increase risks in systemic rheumatic diseases.
- If you plan to become pregnant, wait until your disease has been quiet for at least six months. Meet with your doctor to review your health, medicines, and past pregnancies.
Tip: Keep a symptom diary. Write down any new symptoms or changes. This helps your doctor track your condition and adjust your care.
For Clinicians
When you see a positive anti ro antibody result, clear communication is key. You help your patient understand what the test means and what comes next.
- Use clear, simple language when explaining results. Avoid medical jargon that may confuse your patient.
- Work closely with laboratory staff to confirm the accuracy of the test. Standardized reporting helps prevent misinterpretation.
- Make sure test reports use unambiguous terms. Confusing designations can lead to misdiagnosis or improper management.
- Assess your patient for signs of connective tissue disease or other systemic rheumatic diseases. Review their autoantibody profile, current symptoms, and medical history.
- Discuss lifestyle changes and preventive steps. Encourage sun protection, healthy eating, exercise, and smoking cessation.
- For patients considering pregnancy, review disease activity, medications, and previous obstetric outcomes. Plan care to reduce risks for both mother and baby.
Note: Early and clear guidance supports better outcomes for patients living with autoimmunity.
Understanding the anti ro antibody helps you and your doctor make better decisions about your health. Open conversations with your healthcare team lead to improved care and treatment choices.
| Key Point | Description |
|---|---|
| Regular Checkups | Help track disease changes and catch new symptoms early. |
| Skin and Eye Care | Important for those with dryness or rashes. |
| Ongoing Monitoring | Needed because new autoimmune diseases can develop. |
- Learning about autoimmunity supports early detection and guides your treatment.
- Tracking your antibody levels helps you and your doctor manage your condition.
FAQ
What does a positive anti-Ro antibody test mean for you?
A positive test shows your immune system makes antibodies against your own cells. You may have a higher risk for autoimmune diseases like Sjögren’s syndrome or lupus. Your doctor will check your symptoms and may order more tests.
Can you have anti-Ro antibodies without having an autoimmune disease?
Yes, some healthy people have anti-Ro antibodies. This does not always mean you have a disease. Your doctor will look at your health history and symptoms before making a diagnosis.
How often should you repeat anti-Ro antibody testing?
You usually do not need frequent repeat tests unless your symptoms change or your doctor wants to monitor your condition. Regular checkups help track your health and catch new problems early.
What should you do if you plan to get pregnant and have anti-Ro antibodies?
Talk with your doctor before pregnancy. You may need special monitoring for you and your baby. Early planning helps lower risks and keeps you both safer.