News & Events
A Step-by-Step Guide to Detecting Anti-Smith Antibodies
You can detect anti smith antibody by using specialized lab tests, such as the SmD3 peptide-based ELISA. This test shows higher specificity than older methods and helps you tell systemic lupus erythematosus apart from mixed connective tissue disease. Doctors consider anti-Smith antibodies key markers for these conditions. Before you test for anti-Smith antibodies, you usually need a positive ANA result. Early and accurate detection helps guide both diagnosis and prognosis.
Key Takeaways
- Anti-Smith antibodies are crucial for diagnosing systemic lupus erythematosus (SLE). A positive test indicates a higher likelihood of SLE, helping doctors confirm the disease.
- Always start with an antinuclear antibody (ANA) test before testing for anti-Smith antibodies. A positive ANA result is necessary to justify further testing.
- Use ELISA or immunoblotting methods for accurate detection of anti-Smith antibodies. These methods provide reliable results and are preferred over older techniques.
- Monitor anti-Smith antibody levels to track disease activity in SLE patients. Changes in antibody levels can indicate worsening or improving symptoms.
- Combine anti-Smith antibody results with clinical findings for the best diagnosis. This approach ensures a comprehensive understanding of the patient’s condition.
Anti-Smith Antibody Overview
What Is Anti-Smith Antibody?
You may hear about anti-Smith antibodies when learning about autoimmune diseases. These antibodies target a group of proteins inside the cell nucleus. Scientists call these proteins the Smith antigen. The Smith antigen forms a complex with small nuclear RNAs, which help process genetic information. Anti-Smith antibodies do not focus on just one protein. Instead, they bind to several proteins in the Sm core, including B/B’, D1, D2, D3, E, F, and G. Each of these proteins shares special sequence motifs called Sm1 and Sm2. You can see the main features of anti-Smith antibodies in the table below:
| Characteristic/Target | Description |
|---|---|
| Smith Antigen | A nuclear nonhistone protein complexed with small nuclear RNAs (snRNAs) U1, U2, U4–6, and U5. |
| Immune Response | Multiple antibodies bind to multiple protein antigens, indicating a complex antibody system rather than a single antibody. |
| Target Proteins | Primary targets include Sm core proteins B/B’, D1, D2, D3, E, F, and G, which share common sequence motifs Sm1 and Sm2. |
| Diagnostic Relevance | Anti-Sm antibodies are highly diagnostic of systemic lupus erythematosus (SLE). |
You can trace the discovery of anti-Smith antibodies back to 1966. Researchers found these antibodies in a patient named Stephanie Smith. This discovery changed how doctors diagnose autoimmune diseases. Over time, new testing methods such as indirect immunofluorescence and immunoassays improved accuracy.
Association with SLE and MCTD
You will find anti-Smith antibodies most often in people with systemic lupus erythematosus (SLE). These antibodies help doctors confirm an SLE diagnosis. They rarely appear in other diseases, which makes them very specific markers. Mixed connective tissue disease (MCTD) can also show similar symptoms, but anti-Smith antibodies are much less common in MCTD.
Tip: If you test positive for anti-Smith antibodies, you have a higher chance of certain health problems with SLE. These include:
- Neuropsychiatric symptoms, such as confusion or mood changes.
- Autoimmune hemolytic anemia, where your body destroys its own red blood cells.
- Thrombocytopenia, which means you have fewer platelets and may bleed more easily.
Doctors use anti-Smith antibody results to guide diagnosis and predict possible complications. You can rely on these antibodies as a strong clue for SLE, but not for most other autoimmune conditions.
ANA and Anti-Smith Antibody Testing
ANA Testing as a Prerequisite
You start your journey with ana testing when you suspect an autoimmune disease. The antinuclear antibody test helps you find autoantibodies that attack cell nuclei. In rheumatology, this test is the first step for diagnosing systemic lupus erythematosus (SLE) and other connective tissue diseases. You need a positive ana titer before you move to more specific tests like anti-Smith antibody detection.
Note: Doctors use ana testing because it shows if your immune system makes autoantibodies. A positive result means you should look for more specific markers.
You see the clinical rationale for using ana testing as a prerequisite:
- The antinuclear antibody test is crucial for diagnosing systemic inflammatory autoimmune rheumatic diseases.
- A positive ana test guides you to order tests for specific antibodies, such as anti-Smith.
- Anti-Smith antibodies are very specific for SLE, but only about 20% of SLE patients have them. You need a positive ana titer to justify anti-Smith testing.
In rheumatology, you rely on ana testing to narrow down your diagnosis. You use the ana titer to measure how much autoantibody is present. Higher ana titers often mean more active disease.
Indications for Anti-Smith Antibody Testing
You order anti-Smith antibody testing when you see signs that point to SLE or other autoimmune diseases. The table below shows common reasons for testing:
| Indication | Description |
|---|---|
| Persistent joint pain or swelling | Symptoms that don’t go away and may indicate autoimmune inflammation. |
| Skin rashes | Rashes that worsen after sun exposure, like the butterfly rash in lupus. |
| Long-lasting fever | Fever with no clear cause that doesn’t respond to typical treatments. |
| Unexplained fatigue | Extreme tiredness not related to activity or sleep patterns. |
| Signs of organ involvement | Chest pain from heart or lung inflammation, or kidney problems. |
You follow clinical guidelines in rheumatology to select patients for anti-Smith antibody testing. You look for SLE-specific antibodies, such as anti-dsDNA and anti-Smith. You check if your patient meets at least four out of eleven criteria from the American College of Rheumatology. The presence of anti-Smith antibodies helps you confirm the diagnosis.
🩺 Tip: Always use ana testing first. If you see a positive ana titer and symptoms match, you can move to anti-Smith antibody testing for a more accurate diagnosis.
Sample Collection for Anti-Smith Antibody

Blood Sample Requirements
You need to collect the right type and amount of blood for anti-Smith antibody testing. The test works best with blood drawn into tubes containing ACD-A as the anticoagulant. This helps keep the sample stable and prevents clotting. You should avoid using sodium citrate, EDTA, or heparin because these can affect the results.
Here is a quick guide for blood collection:
| Anticoagulant | Recommended Volume for Adults | Recommended Volume for Children |
|---|---|---|
| ACD-A | 30 mL | 10 mL |
| Sodium Citrate | Not recommended | Not recommended |
| EDTA | Not recommended | Not recommended |
| Heparin | Not recommended | Not recommended |
You should always use the recommended volume. This ensures you have enough serum for accurate testing. If you collect less than the minimum, the lab may not be able to run the test.
Tip: Always label the tube with the patient’s name and the date of collection. This helps prevent mix-ups and keeps the results accurate.
Handling and Transport
Proper handling and transport keep your sample in good condition. After you draw the blood, separate the serum from the cells as soon as possible, ideally within two hours. This step helps prevent changes that could affect the test.
| Specimen Type | Temperature | Time | Special Container |
|---|---|---|---|
| Serum | Refrigerated (preferred) | 21 days | N/A |
| Frozen | 21 days | N/A |
- Separate the serum from the blood cells quickly.
- Transfer at least 1 mL of serum to a standard transport tube. The minimum amount is 0.2 mL.
- Store and ship the sample at refrigerated temperatures.
You can keep the serum at room temperature for up to 48 hours. If you refrigerate it, the sample stays stable for two weeks. Freezing the serum lets you store it for up to one year, but you should avoid thawing and refreezing the sample. This keeps the antibodies stable and helps you get the most accurate results.
Anti-Smith Detection Methods

Detecting anti-smith antibody in the lab involves several reliable methods. You can choose from ELISA, immunoblot techniques, or indirect immunofluorescence. Each method has strengths and limitations. Understanding these helps you select the best approach for your patient.
ELISA for Anti-Smith
ELISA stands for enzyme-linked immunosorbent assay. You use this test to measure anti-smith antibody levels in serum. ELISA kits offer high sensitivity, which means you can detect even small amounts of anti-smith. Some kits reach 100% sensitivity for Sm, RNP, and SSA antigens. Specificity varies, but ELISA remains a top choice for screening.
| Method | Sensitivity | Specificity |
|---|---|---|
| ELISA Kit 2 | 100% | N/A |
| ELISA Kit 3 | 100% | 73% (Sm), 86% (RNP) |
| ELISA Kit 4 | 55% (SSB) | N/A |
You see that ELISA outperforms many older methods. When you need to confirm anti-smith antibody, ELISA gives you reliable results. You can compare ELISA to double immunodiffusion (DID) in the table below.
| Antigen | ELISA Sensitivity | DID Sensitivity | ELISA Specificity | DID Specificity |
|---|---|---|---|---|
| Sm | 100% | N/A | N/A | ≥98% |
| RNP | 100% | N/A | N/A | ≥98% |
| SSA | 100% | N/A | N/A | ≥98% |
| SSB | 100% (Kits 2 & 3) | 64% (Kit 1) | N/A | ≥98% |
Tip: ELISA helps you detect anti-smith quickly and accurately. You can trust this method for routine screening.
Immunoblot Techniques
Immunoblotting allows you to visualize anti-smith antibody binding to specific proteins. You use this method to confirm results from ELISA or to study antibody profiles. Immunoblotting shows very high sensitivity, but specificity can change depending on the lab.
| Technique | Sensitivity | Specificity |
|---|---|---|
| Immunoblotting | Very sensitive | Varies by lab |
| Immunoprecipitation | Very sensitive | Gold standard |
| Immunodiffusion | Less sensitive | Varies |
| Passive hemagglutination | Less sensitive | Varies |
| Counterimmunoelectrophoresis | Less sensitive | Varies |
You may use immunoprecipitation if you need the gold standard for anti-smith detection. Immunoblotting works well for research and confirmation. You should remember that lab technique affects accuracy.
Indirect Immunofluorescence
Indirect immunofluorescence (IIF) uses fluorescent dyes to detect anti-smith antibody. You apply patient serum to cells, then add a dye-labeled antibody. If anti-smith is present, you see a glowing pattern under the microscope.
- IIF shows limited sensitivity for anti-Rib-P antibodies (less than 30%).
- ELISA and immunoblot methods provide higher sensitivity and reliability.
- IIF may not work well for screening anti-smith antibody.
You may use IIF for general ANA screening, but you should rely on ELISA or immunoblot for anti-smith detection. IIF can miss cases due to low sensitivity.
Note: You get the most accurate results for anti-smith antibody when you use ELISA or immunoblotting. IIF works best as a first step, not for confirmation.
Step-by-Step Anti-Smith Antibody Detection
Detecting anti smith antibody in your patients involves careful planning and attention to detail. You need to follow each step closely to ensure accurate results. This guide will help you understand what to do before, during, and after the testing process.
Pre-Analytical Steps
You begin with the pre-analytical phase. This stage sets the foundation for reliable anti-sm antibody testing. Start by confirming that your patient meets the criteria for testing. Look for a positive ANA result and clinical signs that suggest SLE or related diseases.
Follow these steps to prepare your sample:
- Collect the correct blood volume using ACD-A tubes. Avoid other anticoagulants.
- Label each tube with the patient’s name and collection date.
- Separate the serum from blood cells within two hours. This step prevents changes that could affect anti-sm antibody detection.
- Store the serum at refrigerated temperatures if you plan to test within two weeks. Freeze the sample if you need to store it longer.
🧪 Tip: Always double-check patient identification before collecting samples. Mistakes at this stage can lead to incorrect results.
You should also review the patient’s medication history. Some drugs can interfere with anti-sm antibody testing. If possible, collect samples when the patient is not taking immunosuppressive medications.
Analytical Procedures
The analytical phase is where you actually detect anti smith antibody in the lab. You have several methods to choose from, but ELISA and immunoblotting are the most common for anti-sm antibody testing.
Here is a typical workflow for anti-sm antibody detection:
- Prepare your reagents and calibrate your equipment according to the manufacturer’s instructions.
- Add patient serum to the test wells or strips.
- Incubate the samples for the recommended time. This allows any anti-sm antibody present to bind to the target antigens.
- Wash away unbound substances to reduce background noise.
- Add detection reagents, such as enzyme-linked antibodies or fluorescent markers.
- Measure the signal using a plate reader or fluorescence microscope.
You need to include positive and negative controls in every run. Controls help you spot errors and ensure your anti-sm antibody testing is working correctly.
⚠️ Common Pitfalls to Avoid:
- Inter-observer variability: Different readers may interpret results differently.
- Inter-assay variability: Results can change between labs, making it hard to compare antibody levels.
- Subjective interpretation: Some tests rely on visual judgment, which can lead to mistakes.
- False positives: Using the wrong serum dilution can cause incorrect positive results.
You can reduce these risks by following standard operating procedures and using automated systems when possible. Training your staff regularly also helps maintain consistency in anti-sm antibody testing.
Post-Analytical Considerations
After you finish the analytical phase, you must validate and report your results. This step is just as important as the earlier ones. Accurate reporting ensures that clinicians can make the right decisions for their patients.
Here is a table that summarizes key post-analytical considerations:
| Consideration | Description |
|---|---|
| Timely Delivery | Results must be delivered promptly to support clinical decision-making, especially in acute conditions. |
| Clarity in Reporting | Reports should be clear, stating the assay type, test result, and autoantibody titer to avoid confusion. |
| Standardized Procedures | Laboratories should follow standardized procedures to ensure accuracy and reliability of test results. |
| Understanding Diagnostic Utility | Clinicians must understand the diagnostic implications of test results in the context of biological variations. |
You should always deliver anti smith antibody results quickly, especially if your patient has severe symptoms. Make sure your report clearly states the type of assay used, the result, and the anti-sm antibody titer. Use standardized language and formats to avoid confusion.
📋 Note: Always review your results in the context of the patient’s clinical picture. Anti-sm antibody testing is highly specific, but only a small percentage of SLE patients test positive. Combine laboratory data with clinical findings for the best diagnosis.
You can improve reliability by participating in external quality assessment programs. These programs help you compare your results with other labs and identify areas for improvement in anti-sm antibody testing.
Interpreting Anti-Smith Antibody Results
Positive vs Negative Findings
When you receive a result for anti-Smith antibody testing, you need to understand what it means for your patient. If you see a positive ana and a positive anti-Smith antibody result, you can feel confident about the diagnosis of lupus. This antibody appears almost only in lupus patients. You rarely find it in other diseases. A positive ana and a positive anti-Smith antibody result together point strongly toward lupus.
If you see a negative result for anti-Smith antibody, you should not rule out lupus. Many patients with lupus have a positive ana but do not have anti-Smith antibodies. You need to look at the whole clinical picture and other test results before making a diagnosis.
Here is a table that helps you interpret the findings:
| Interpretation of Anti-Smith Antibody Findings | Description |
|---|---|
| Positive Finding | Indicates a higher likelihood of systemic lupus erythematosus (SLE) diagnosis, as this antibody is found almost exclusively in lupus patients. |
| Negative Finding | Does not rule out lupus, as not all lupus patients test positive for this antibody. |
📝 Tip: Always check for a positive ana before ordering anti-Smith antibody testing. Use the result as part of a bigger diagnostic strategy.
Sensitivity and Specificity
You need to know how well anti-Smith antibody testing works. Sensitivity tells you how often the test finds the antibody in people who have lupus. Specificity tells you how often the test gives a negative result in people who do not have lupus. Most anti-Smith antibody tests show high specificity but low sensitivity. This means the test is very good at confirming lupus when the antibody is present, but it misses many cases because not all lupus patients have this antibody.
Look at the table below to compare different assays:
| Assay Type | Sensitivity (%) | Specificity (%) |
|---|---|---|
| Euroimmun anti-Sm ELISA | 10 | 94 |
| QuantaLite Sm (INOVA) | 10 | 90 |
| Varelisa ReCombi ANA profile | 12 | 88 |
| QuantaPlex Sm (INOVA) | 10 | 94 |
| SmD3 peptide-based ELISA | 12 | 100 |
You can see that sensitivity stays low, around 10-12%. Specificity is much higher, reaching up to 100% with the SmD3 peptide-based ELISA. This means you can trust a positive result, especially if you already have a positive ana.
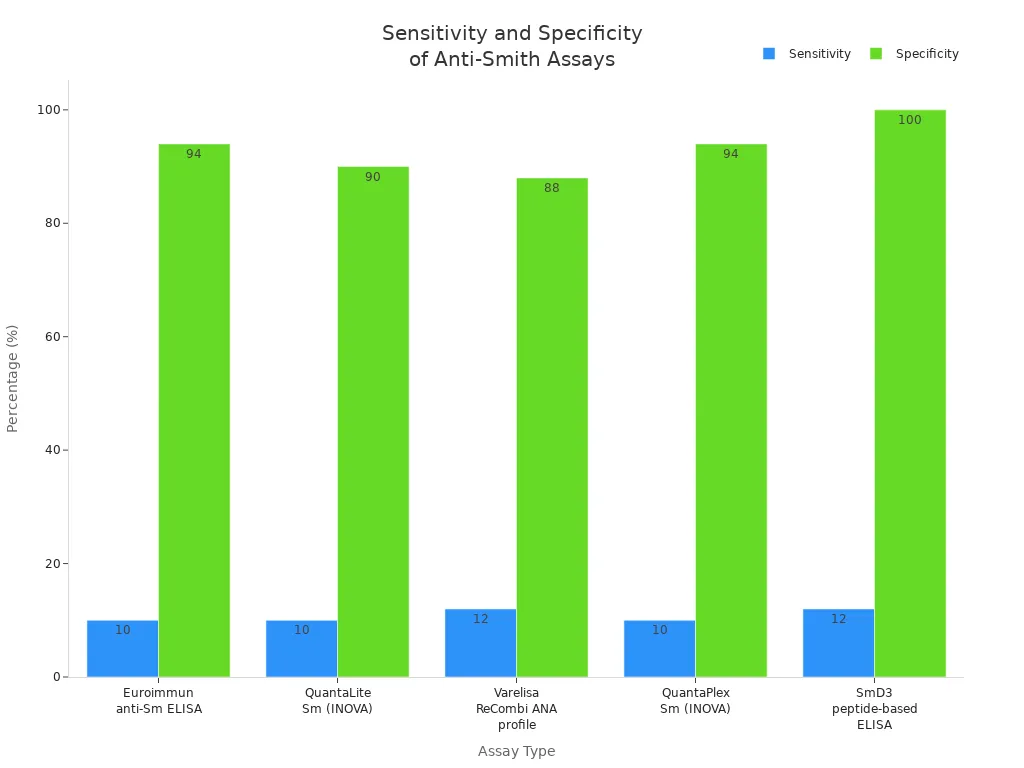
📊 Note: Always use anti-Smith antibody testing after a positive ana. High specificity helps you confirm lupus, but low sensitivity means you need other tests and clinical signs for a complete diagnosis.
Clinical Implications
You use anti-Smith antibody results to guide your decisions in patient care. If you see a positive ana and a positive anti-Smith antibody result, you can move forward with a lupus diagnosis. This antibody helps you confirm the disease and plan treatment. You also use the result to predict possible complications. Anti-Smith antibodies often appear months before diagnosis, so you can catch lupus early if you test at the right time.
Here is a table that shows how anti-Smith antibody results help you manage patients:
| Evidence Type | Description |
|---|---|
| Autoantibody Role | Anti-Smith antibodies are associated with the development of systemic lupus erythematosus (SLE) and can guide clinical decisions. |
| Prognostic Value | Specific autoantibody markers help in assessing prognosis and tailoring treatment strategies. |
| Personalized Treatment | Biomarkers enable personalized therapy choices, improving treatment safety and efficacy. |
You can use anti-Smith antibody results to:
-
Confirm lupus diagnosis when you see a positive ana and matching symptoms.
-
Assess prognosis and predict disease activity.
-
Choose personalized treatments that fit your patient’s needs.
-
Some autoantibodies, such as anti-Ro and anti-La, can appear years before diagnosis.
-
Anti-Smith antibodies usually show up months before diagnosis, often with symptoms.
-
Knowing when these antibodies appear helps you diagnose and manage lupus early.
🩺 Tip: Always combine anti-Smith antibody results with a positive ana and clinical findings. This approach helps you make the best decisions for your patient.
Clinical Significance of Anti-Smith Antibody
Role in SLE Classification
You play a key role in diagnosing autoimmune diseases like sle and mctd. Anti-Smith antibodies help you classify sle because they show high specificity for this disease. You find these antibodies in about 5% to 30% of sle patients. You may detect them before you make a formal diagnosis. When you see these antibodies, you know the patient likely has sle, not mixed connective-tissue disease or other autoimmune diseases. Even though no standard test exists for screening, you rely on anti-Smith antibodies as a strong marker. Their presence helps you separate sle from other autoimmune diseases with similar symptoms.
Note: Anti-Smith antibodies rarely appear in other autoimmune diseases, so their presence gives you confidence in your sle diagnosis.
Prognostic Value
You use anti-Smith antibodies to predict how sle may progress in your patients. These antibodies often signal a higher risk for early poor outcomes, especially in patients with lupus nephritis. If you see a patient who needs immunosuppressant medication more than three months after a kidney biopsy, you know the prognosis is less favorable. You should watch for these symptoms and adjust treatment plans as needed.
- The presence of anti-Smith antibodies links to:
- Early poor outcomes in lupus nephritis
- The need for ongoing immunosuppressive therapy
- More severe autoimmune symptoms
| Finding | Description |
|---|---|
| Correlation with SLEDAI | Serum anti-Sm antibody level at diagnosis was significantly correlated with SLEDAI (P = 0.003). |
| Higher SLEDAI in Patients | Patients with anti-Sm antibodies at 12 months had higher SLEDAI and anti-dsDNA levels (P = 0.002). |
| Changes Over Time | Changes in anti-Sm antibody levels over 12 months correlated with alterations in SLEDAI (P = 0.029). |
Disease Activity and Monitoring
You monitor anti-Smith antibody titer to track sle activity in your patients. The titer often rises when symptoms worsen and falls when symptoms improve. You see a strong link between titer and the SLE Disease Activity Index (SLEDAI). If you notice the titer increasing, you should check for new or worsening autoimmune symptoms. You also compare the titer with anti-dsDNA levels to get a full picture of disease activity. This approach helps you adjust treatment and monitor progress in sle and mctd.
🩺 Tip: Regularly check anti-Smith antibody titer in patients with sle or mctd. This helps you spot changes in autoimmune disease activity and respond quickly to new symptoms.
Next Steps After Anti-Smith Antibody Detection
Impact on Diagnosis
When you detect anti-Smith antibodies, you gain a powerful tool for diagnosing systemic lupus erythematosus (SLE). These antibodies show high specificity for SLE, which means you can use them to confirm the disease and separate it from other autoimmune disorders. You also use the Anti-Sm Antibody test to monitor disease progression in patients who already have a diagnosis. The table below highlights how anti-Smith antibodies help you in the diagnostic process:
| Evidence Type | Description |
|---|---|
| Specificity for SLE | Anti-Smith antibodies are highly specific for SLE, aiding in diagnosis. |
| Monitoring Disease Progression | The Anti-Sm Antibody test is useful for monitoring disease progression in diagnosed patients. |
| Distinguishing from Other Disorders | The presence of these antibodies helps differentiate SLE from other autoimmune diseases. |
🩺 Tip: Always combine anti-Smith antibody results with clinical findings and other lab tests for the most accurate diagnosis.
Treatment Considerations
After you confirm the presence of anti-Smith antibodies, you need to plan treatment based on disease severity and risk factors. You should monitor for lupus nephritis, especially in patients at high risk. You also manage complications that may arise from SLE. Treatment often starts with an induction phase using cyclophosphamide or mycophenolate along with high-dose glucocorticoids. You then move to maintenance therapy with mycophenolate or azathioprine. The table below summarizes key treatment considerations:
| Treatment Considerations for Positive Anti-Smith Antibodies |
|---|
| Monitoring for Lupus Nephritis |
| Management of Complications |
| Therapy Based on Disease Severity |
⚠️ Note: Adjust therapy as needed based on your patient’s response and any new symptoms.
Follow-Up Recommendations
You need to follow a structured protocol to monitor patients after anti-Smith antibody detection. At each visit, you should review medical history, perform a physical exam, and evaluate disease activity. Annually, you assess organ damage and screen for other health problems. If your patient takes hydroxychloroquine, schedule an eye exam at baseline and every six months. Order lab tests as needed to track disease changes. The table below outlines recommended follow-up steps:
| Follow-Up Protocols for SLE Patients | Frequency |
|---|---|
| Medical history evaluation | At each visit |
| Physical examination | At each visit |
| Disease activity evaluation | At each visit |
| Damage evaluation | Annually |
| Comorbidity screening | Annually |
| Ocular examination (hydroxychloroquine) | Baseline, then every 6 months |
| Laboratory tests | As needed |
💬 Tip: Communicate clearly with your patients about their test results and next steps. Encourage questions and provide written information to help them understand their care plan.
Accurate anti-Smith antibody detection helps you improve patient outcomes in autoimmune diseases. You see higher disease activity and risk for kidney problems when these antibodies are present. The table below shows key findings:
| Description | Findings |
|---|---|
| Increased autoantibody positivity | Higher SLE activity |
| Anti-Smith antibodies | More lymphopenia, hypocomplementemia |
| Urinary anti-Smith titers | 100% renal involvement |
You should always start with ANA testing before moving to anti-Smith antibody tests. Use best practices to guide diagnosis and patient care.
FAQ
What does a positive anti-Smith antibody test mean?
A positive anti-Smith antibody test means you likely have systemic lupus erythematosus (SLE). This antibody is very specific for SLE. You rarely see it in other diseases.
Can you have lupus without anti-Smith antibodies?
Yes, you can have lupus without anti-Smith antibodies. Only about 20% of people with lupus test positive for this antibody. Doctors use other tests and symptoms to help confirm the diagnosis.
How long does it take to get anti-Smith antibody test results?
Most labs provide results within a few days. Some specialized tests may take up to one week. You should ask your healthcare provider about the expected timeline.
Do medications affect anti-Smith antibody test results?
Some medications, especially immunosuppressants, can lower antibody levels. You should tell your doctor about all medicines you take. This helps ensure accurate test results.
Why do you need an ANA test before anti-Smith antibody testing?
Doctors use the ANA test first because it checks for general autoimmunity. If you have a positive ANA, you may need more specific tests, like anti-Smith antibody testing, to confirm a diagnosis.