News & Events
What Is Anticentromere Antibody and How Does It Help Diagnose Autoimmune Diseases

Anticentromere antibody helps you understand the diagnosis of autoimmune diseases. You may find this antibody in several conditions. Most often, doctors see it in systemic sclerosis, especially the limited form called CREST syndrome. You might also see it in diseases like systemic lupus erythematosus, primary biliary cirrhosis, rheumatoid arthritis, and Sjögren’s syndrome. In Sjögren’s syndrome, studies show a prevalence between 3.7% and 8.7%. In systemic sclerosis, it occurs in about 20% to 40% of patients. This antibody gives doctors important clues when they look for signs of autoimmune diseases.
Key Takeaways
- Anticentromere antibodies are crucial for diagnosing autoimmune diseases, especially limited scleroderma and CREST syndrome.
- A positive anticentromere antibody test indicates a higher risk of developing limited scleroderma, guiding doctors in treatment planning.
- The anti-centromere antibody test is highly specific, with a 95% accuracy rate for detecting limited scleroderma, making it a reliable diagnostic tool.
- You do not need to fast before the test, allowing for a normal routine before your blood draw.
- Discuss your test results with your doctor to understand their implications for your health and treatment options.
Anticentromere Antibody Overview
What Is Anticentromere Antibody
You may hear about anticentromere antibody when you learn about scleroderma and other autoimmune diseases. This antibody belongs to a group called autoantibodies. Your immune system makes autoantibodies when it mistakes parts of your own body for harmful invaders. In this case, anticentromere antibodies target the centromere, a special part of your cell’s chromosomes. The centromere helps your cells divide correctly. It contains proteins like CENP-A and connects to microtubules through a structure called the kinetochore. When you have anticentromere antibodies, your immune system attacks this important area.
Note: Doctors often find anticentromere antibodies in people with scleroderma, Sjögren’s syndrome, and primary biliary cholangitis. These antibodies show up as a unique pattern in the anti-nuclear antibody test, which helps doctors spot autoimmune problems.
You can see how these autoantibodies play a role in your body’s defense system, but sometimes they cause trouble by attacking healthy tissues.
Role in Autoimmune Diseases
Anticentromere antibodies are important in the diagnosis and understanding of scleroderma. You may notice that these autoantibodies appear in several autoimmune diseases, but they are most common in scleroderma, especially the limited form. When you have these antibodies, your body may form immune complexes that include nucleic acids. These complexes can activate cells in your blood vessels and cause inflammation. They also trigger fibroblasts, which can lead to thickening and scarring of your skin and organs.
- Anticentromere antibodies may come from nuclear antigens released during cell death.
- These autoantibodies can start a chain reaction that leads to tissue damage in scleroderma.
You might wonder how these antibodies relate to symptoms. In scleroderma, anticentromere antibodies link to limited skin changes, more cases of calcinosis (calcium deposits), and problems with your digestive system. The amount of IgG anticentromere antibody in your blood can show how severe your disease is and how fast it may get worse.
| Antibody Isotype | Odds Ratio | 95% Confidence Interval |
|---|---|---|
| IgG ACA | 2.5 | 1.8 – 3.7 |
| IgM ACA | 1.8 | 1.3 – 2.3 |
| Progression to Definite SSc (IgG) | 4.3 | 1.7 – 10.7 |
You can see that higher levels of IgG anticentromere antibody increase your risk of developing definite scleroderma. The anti-centromere antibody test helps your doctor understand your risk and plan your care.
Anticentromere Antibody Test
Test Procedure
You may need an anti-centromere antibody test if your doctor suspects an autoimmune disease. This test helps you and your doctor find out if your immune system makes antibodies against the centromere part of your chromosomes. You will give a blood sample for the anti-centromere antibody test. The lab uses special methods to look for these antibodies in your blood.
Most labs use indirect immunofluorescence (IFA) or enzyme-linked immunosorbent assay (ELISA) for anti-centromere antibody testing. These methods help doctors see if you have antibodies that target the centromere. You do not need to prepare for the anti-centromere antibody test. You can eat and drink normally before your blood draw.
You may wonder how accurate the anti-centromere antibody test is. Doctors report that the test detects anticentromere antibodies in about 50-90% of patients with limited scleroderma. In patients with the CREST variant, the detection rate is even higher, between 82-96%. The specificity of the anti-centromere antibody test reaches 95%. This means the test rarely gives a false positive result.
- You can expect the anti-centromere antibody test to be very specific for certain autoimmune diseases.
- The test helps your doctor confirm a diagnosis when you have symptoms like skin thickening, Raynaud’s phenomenon, or other signs of systemic sclerosis.
After you give your blood sample, the lab needs time to process your anti-centromere antibody test. The turnaround time depends on the type of test your doctor orders.
| Test Type | Turnaround Time |
|---|---|
| Anticentromere B Antibodies | 1 – 3 days |
| Anti-Centromere Ab by IFA (RDL) | 14 – 21 days |
You may receive your results in a few days or up to three weeks. Your doctor will explain what your anti-centromere antibody test results mean for your health.
When to Order the Test
You should consider anti-centromere antibody testing if you have symptoms that suggest an autoimmune disease. Doctors often order the anti-centromere antibody test when you show signs of systemic sclerosis, Sjögren’s syndrome, or other systemic autoimmune rheumatic diseases. The test helps your doctor decide which type of disease you may have and how to treat you.
| Clinical Scenario | Description |
|---|---|
| Systemic Autoimmune Rheumatic Disease | Evaluating patients with features of systemic autoimmune rheumatic disease, particularly systemic sclerosis, Sjogren’s syndrome, or overlap disease. |
| Phenotypic Stratification | Aiding in the phenotypic stratification of patients with systemic sclerosis (limited cutaneous vs diffuse cutaneous or risk for specific clinical manifestations). |
You may need the anti-centromere antibody test if you have symptoms like tight skin, swollen fingers, or trouble swallowing. The test helps your doctor find out if you have limited or diffuse cutaneous systemic sclerosis. You may also need anti-centromere antibody testing if you have unexplained symptoms that suggest an overlap of autoimmune diseases.
Doctors use the anti-centromere antibody test to guide treatment and monitor your disease. You may need repeat anti-centromere antibody testing if your symptoms change or if your doctor wants to check your risk for certain complications.
You may want to know about the cost of the anti-centromere antibody test. The test usually costs about $139.00 USD. Many insurance plans, including HSA and FSA, approve coverage for anti-centromere antibody testing.
| Cost of Test | Insurance Coverage |
|---|---|
| $139.00 USD | HSA and FSA Approved |
You do not need to worry about special preparation for the anti-centromere antibody test. You can go to your appointment and have your blood drawn without changing your routine. Your doctor will help you understand the results and what they mean for your health.
Tip: If you have symptoms of an autoimmune disease, ask your doctor about anti-centromere antibody testing. Early testing for anticentromere antibodies can help you get the right diagnosis and treatment.
Test Results Interpretation

Positive and Negative Results
When you receive your anticentromere antibody test results, you want to know what they mean for your health. A positive aca result often points to limited scleroderma or CREST syndrome. Doctors use this finding to predict your disease pattern and help guide your care. If you have elevated levels of anti-centromere antibodies, you may face a higher chance of developing symptoms linked to limited scleroderma. In fact, studies show that anticentromere antibodies appear in about 20% to 40% of patients with limited cutaneous systemic sclerosis. You may also see these antibodies in other autoimmune diseases, but the rate is much lower—less than 3% among positive ANA cases.
A negative aca test means that these antibodies do not show up in your blood. You should know that a negative result does not rule out autoimmune disease. Some people with scleroderma or similar conditions may still have symptoms even if their anticentromere antibody test is negative. Your doctor may order more tests to look for other causes of your symptoms.
Tip: Always discuss your anticentromere antibody test results with your doctor. Your symptoms and medical history matter just as much as your lab results.
Associated Conditions
You may wonder which conditions link to a positive anticentromere antibody test. The most common is limited cutaneous systemic sclerosis. This test helps doctors confirm the diagnosis and predict your risk for certain complications. You may also see anticentromere antibodies in other autoimmune diseases, but the connection is weaker.
Here are some conditions often found with a positive anticentromere antibody test:
- Limited cutaneous systemic sclerosis (lcSSc)
- CREST syndrome
- Sjögren’s syndrome
- Primary biliary cholangitis
You may also notice other health issues in people with positive test results:
- Autoimmune diseases: 38.2%
- Neurological diseases: 15.5%
- Hemopathies: 8.3%
- Cancer: 10.9% (including lung and breast cancer)
Doctors use the anticentromere antibody test to help identify these conditions and guide your treatment plan. If you have symptoms or risk factors, this test can be a valuable tool for your diagnosis.
Anti-Centromere Antibody in Autoimmune Disease Diagnosis
Diagnostic Value
You may wonder how the anti-centromere antibody helps your doctor diagnose and monitor autoimmune conditions. This antibody plays a key role in identifying scleroderma, especially limited cutaneous scleroderma and CREST syndrome. When you test positive for anti-centromere antibody, your doctor can use this information to guide crest syndrome diagnosis and predict your disease course.
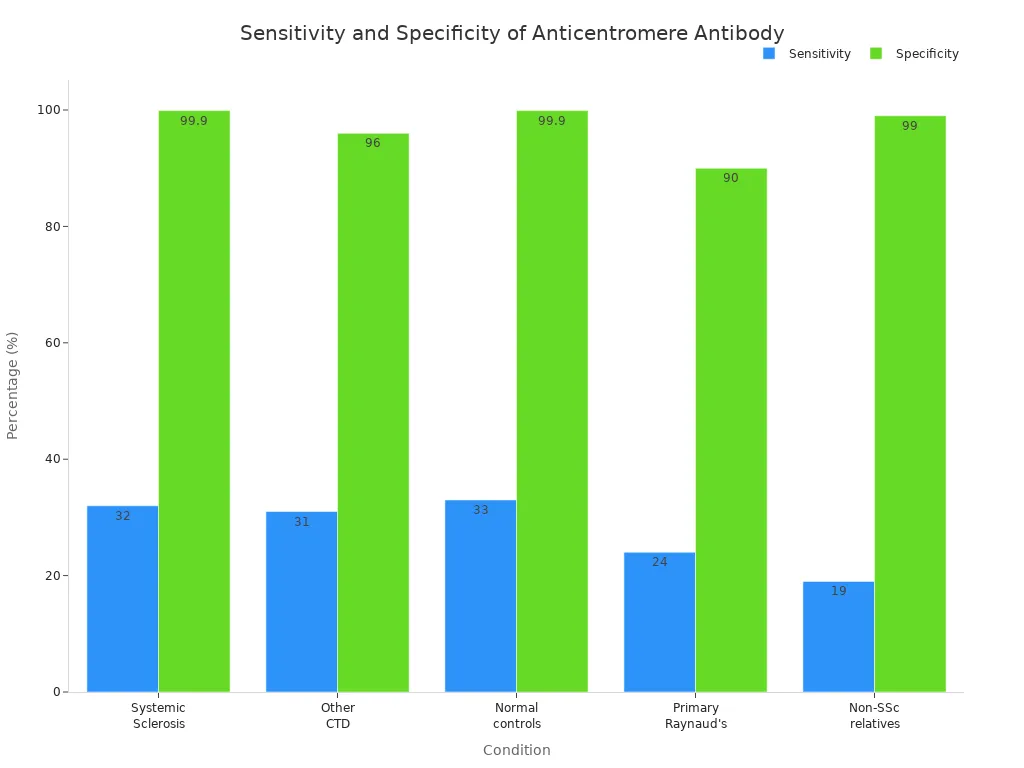
Doctors rely on the anti-centromere antibody test because it shows high specificity for scleroderma. You can see how well the test works in the table below:
| Condition | Sensitivity (%) | Specificity (%) |
|---|---|---|
| Systemic Sclerosis (overall) | 32 | 99.9 |
| Limited cutaneous SSc (CREST) | 57 | N/A |
| Other connective tissue diseases | 31 | 95-97 |
| Normal controls | 33 | 99.9 |
| Primary Raynaud’s phenomenon | 24 | 90 |
| Non-SSc relatives | 19 | >99 |
You can see that the anti-centromere antibody test is very specific for scleroderma and crest syndrome diagnosis. This means you are unlikely to get a false positive result. The sensitivity is higher for limited cutaneous scleroderma, which helps your doctor confirm the diagnosis when you have symptoms of crest syndrome.
If you have limited cutaneous scleroderma, a positive anti-centromere antibody test can help your doctor predict your prognosis. You may have a milder disease course and a better chance of long-term survival. The table below shows how the presence of anticentromere antibody affects survival rates:
| Antibody Type | 10-Year Survival Rate |
|---|---|
| Anticentromere Antibodies | 93% |
| Anti-Scl-70 Antibodies | 66% |
You can see that patients with anticentromere antibody have a much higher survival rate than those with anti-Scl-70 antibodies. This means you may experience fewer severe complications and a better overall outcome.
- The presence of anti-centromere antibody is linked to a lower risk of developing serious lung problems, such as interstitial lung disease.
- Early detection of anticentromere antibody can help your doctor identify patients who are less likely to develop severe organ involvement.
- You may benefit from early testing, which allows your doctor to plan your care and monitor your health more closely.
Tip: If you have symptoms of crest syndrome or limited cutaneous scleroderma, ask your doctor about anti-centromere antibody testing. Early diagnosis can help you avoid complications and improve your quality of life.
Limitations
You should know that the anti-centromere antibody test has some limitations. While it helps with crest syndrome diagnosis and limited cutaneous scleroderma, it does not work perfectly for every autoimmune disease diagnosis.
- The sensitivity of the test is not very high for all forms of scleroderma. Some patients with scleroderma may test negative for anti-centromere antibody.
- The test depends on subjective interpretation. Lab technicians must recognize patterns, which can lead to errors if they lack experience.
- You may need highly trained personnel to perform and interpret the test accurately.
- Sometimes, the test detects multiple autoantibodies that show the same pattern. This can make it hard for your doctor to pinpoint the exact autoimmune disease.
- Certain autoantigens may not show up well in the cells used for testing. This can lower the accuracy of the results.
You may also see anti-centromere antibody in other autoimmune diseases, but the connection is weaker. The test cannot always tell the difference between limited cutaneous scleroderma and other conditions. Your doctor may need to order more tests to confirm your diagnosis.
Note: Always talk to your doctor about your test results. The anti-centromere antibody test is just one part of autoimmune disease diagnosis. Your symptoms, medical history, and other lab tests matter too.
You should remember that early detection of anticentromere antibody can help your doctor identify patients at lower risk for severe complications. However, the test does not replace a full clinical evaluation. Your doctor uses all available information to diagnose and monitor autoimmune conditions and to plan your treatment.
You can see how the anticentromere antibody test helps doctors diagnose autoimmune diseases. This test is reliable and often used when scleroderma is suspected.
- Doctors find these antibodies in about 22 to 36 percent of people with scleroderma.
- Their presence links to symptoms like Raynaud’s phenomenon and CREST syndrome.
- ELISA and immunofluorescence tests both give accurate results.
Always talk to your healthcare provider about your results. Your doctor can help you understand what your test means for your health.
FAQ
What does a positive anticentromere antibody test mean?
A positive test means your immune system makes antibodies against the centromere. You may have a higher chance of having limited scleroderma or CREST syndrome. Your doctor uses this result to help guide your diagnosis and care.
Can you have autoimmune disease with a negative anticentromere antibody test?
Yes, you can. A negative result does not rule out autoimmune disease. Some people with scleroderma or similar conditions do not have these antibodies. Your doctor may order more tests to find the cause of your symptoms.
How accurate is the anticentromere antibody test?
The test is very specific. It gives a true positive result in about 95% of cases with limited scleroderma. False positives are rare. Sensitivity is lower, so some people with the disease may test negative.
Do you need to fast before the anticentromere antibody test?
No, you do not need to fast. You can eat and drink as usual before your blood draw. The test only needs a small blood sample.
What symptoms suggest you should get tested for anticentromere antibodies?
You should get tested if you have symptoms like tight skin, swollen fingers, Raynaud’s phenomenon, or trouble swallowing. These signs may point to scleroderma or another autoimmune disease.

