News & Events
Cardiolipin Antibody: The Hidden Clotting Story Unveiled

Cardiolipin antibodies are proteins your immune system can make that target a specific part of your cells. These antibodies sometimes relate to blood clotting problems, but most people who have cardiolipin antibody in their blood do not face a higher risk of clots. Studies show that even when you test positive for these antibodies, you likely will not develop clotting disorders.
If you worry about clotting or have autoimmune conditions, learning about these antibodies helps you understand your health better.
Key Takeaways
- Cardiolipin antibodies can indicate a risk for blood clots, but most people with these antibodies do not develop clotting disorders.
- Testing for anticardiolipin antibodies is important if you have unexplained blood clots, recurrent miscarriages, or symptoms of autoimmune diseases.
- A positive test result does not confirm a diagnosis of antiphospholipid syndrome; further testing and clinical evaluation are necessary.
- Lifestyle changes, such as avoiding smoking and maintaining a healthy diet, can help lower your risk for blood clots.
- Regular monitoring and communication with your healthcare provider are essential for managing your health if you have cardiolipin antibodies.
Anticardiolipin Antibodies Overview
Definition
You may hear your doctor talk about anticardiolipin antibodies when discussing blood tests for clotting problems. These antibodies belong to a group called antiphospholipid antibodies. Your immune system makes them when it mistakenly targets certain fats, called phospholipids, found in your cell membranes. When you have these antibodies, your body may react to its own cells, which can sometimes lead to health issues.
Types (IgG, IgM)
Doctors classify anticardiolipin antibodies into different types. The main types are IgG, IgM, and IgA. Each type depends on a protein called β2-glycoprotein. You can see the classification in the table below:
| Type | Dependency |
|---|---|
| IgM | β2-glycoprotein dependent |
| IgG | β2-glycoprotein dependent |
| IgA | β2-glycoprotein dependent |
| β2-glycoprotein independent | |
| Assayed in syphilis |
Doctors often focus on IgG and IgM types during clinical testing. These types help guide your doctor in understanding your risk for certain conditions.
- IgG anticardiolipin antibodies appear more often in patients with advanced disease stages, especially in some cancers like NHL.
- IgM anticardiolipin antibodies show up less often but still play a role in clinical decisions.
- High levels of these antibodies may signal a higher risk for serious health problems.
Role in Clotting
Anticardiolipin antibodies are a type of antiphospholipid antibody. They target and damage phospholipids in healthy cells. This damage can disrupt normal cell functions. When this happens, your risk for abnormal blood clot formation increases. Doctors call this group of problems antiphospholipid syndrome. If you have high levels of these antibodies, your clinical team may watch you closely for signs of clotting.
Note: Not everyone with these antibodies will develop clots, but your clinical risk may rise if you have other factors.
Doctors use clinical tests to measure these antibodies and other phospholipid antibodies. These results help guide your care and treatment. Understanding your levels can help you and your clinical team make informed decisions about your health.
Cardiolipin Antibody Testing

When Testing Is Needed
You may wonder when your doctor recommends testing for anticardiolipin antibodies. Doctors often order this testing if you have symptoms that suggest blood clotting problems. You may need testing if you have had unexplained blood clots, strokes, or repeated miscarriages. Doctors use anticardiolipin antibodies testing to help diagnose antiphospholipid syndrome (APS). APS can cause serious health issues, including recurrent thrombosis and pregnancy loss.
Sometimes, testing can give false-positive results. Your doctor may need more than one test to confirm a diagnosis.
Common reasons for anticardiolipin antibodies testing include:
- Unexplained blood clots in veins or arteries
- Recurrent miscarriages
- Suspected autoimmune diseases like lupus
- Symptoms of APS
How the Test Works
Doctors use laboratory methods to detect anticardiolipin antibodies in your blood. The most common methods include ELISA and CLIA-based immunoassays. These tests measure the levels of IgG and IgM anticardiolipin antibodies. You may see your doctor use both manual and automated methods for testing. The accuracy of these tests varies. The table below shows how well different methods work:
| Method | Sensitivity (%) | Specificity (%) |
|---|---|---|
| EliA aCL IgG | 69.4 | 81.9 |
| EliA aCL IgM | 64.5 | 86.7 |
| Anti-beta2-GPI IgG | 64.5 | 98.8 |
| Anti-beta2-GPI IgM | 53.2 | 92.8 |
| Combined aCL and anti-beta2-GPI | 85.7 | 90.4 |
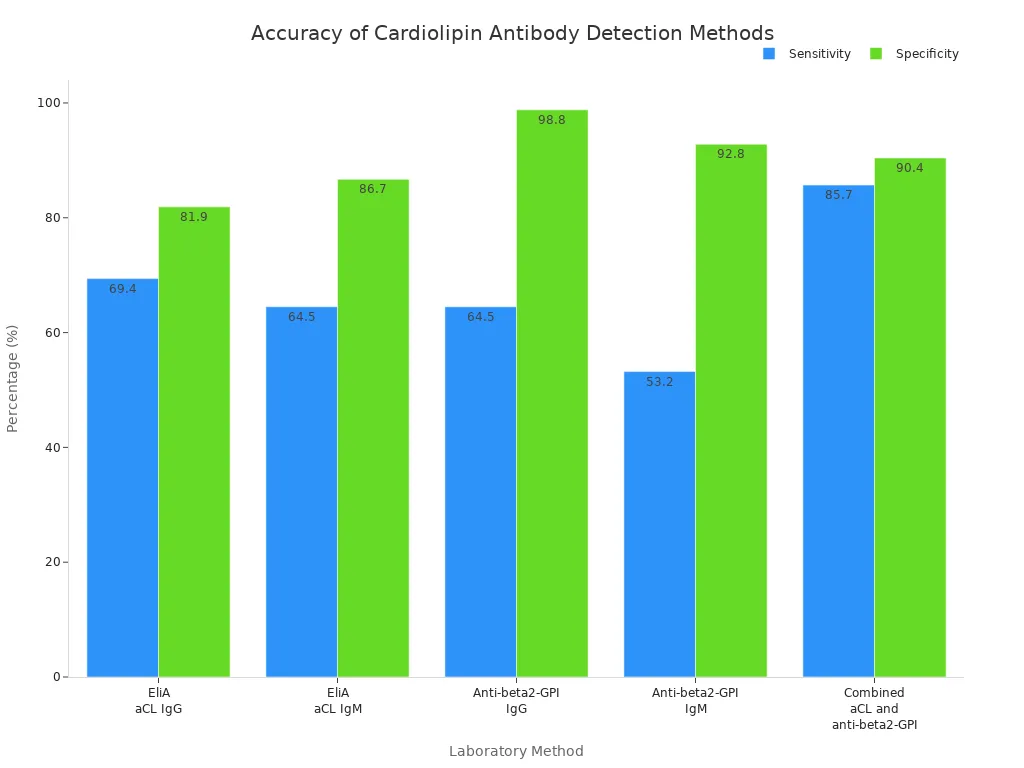
Doctors may choose the method based on your symptoms and the need for accurate results. Testing for anticardiolipin antibodies helps your doctor decide on the best care plan for you.
What to Expect
During anticardiolipin antibodies testing, a nurse or technician draws blood from your arm or hand. You may feel a small sting or pain when the needle goes in. Some people feel lightheaded or notice bruising after the blood draw. The site may be sore for a short time. The table below explains each step:
| Step | Description |
|---|---|
| Blood Draw | A needle is used to draw blood from a vein in your arm or hand. |
| Risks | Potential risks include bleeding, infection, bruising, and feeling lightheaded. |
| Sensation | Patients may feel a slight sting or pain when the needle pricks their arm or hand. |
| Aftercare | The site may be sore after the procedure. |
If your anticardiolipin antibodies testing result is positive, you may need a follow-up test. Doctors often wait six weeks before repeating the test. This helps confirm if the antibodies stay in your blood. If you have lupus or other autoimmune conditions, repeat testing is important for accurate diagnosis.
Your doctor will explain your results and guide you on the next steps.
Interpretation of Test Results
Positive, Negative, Borderline
When you receive your anticardiolipin antibodies testing report, you will see results described as negative, weak positive, or positive. These categories help you and your doctor understand your clinical risk and guide your diagnosis. The table below shows the reference ranges for IgG and IgM anticardiolipin antibodies:
| Antibody Type | Negative (U/mL) | Weak Positive (U/mL) | Positive (U/mL) |
|---|---|---|---|
| IgG ACA | <10 | 10–40 | >40 |
| IgM ACA | <10 | 10–40 | >40 |
If your result falls below 10 U/mL, you have a negative test. Results between 10 and 40 U/mL are considered weak positive or borderline. Values above 40 U/mL are positive. You may notice that borderline results can change over time. Studies show that some patients with systemic lupus erythematosus convert from positive to negative or vice versa on repeat testing. This fluctuation means your clinical team may recommend repeat testing to confirm your diagnosis.
- Some patients with borderline anticardiolipin antibodies results later test negative.
- Others may shift from negative to positive after follow-up testing.
- Fluctuating levels can complicate your clinical interpretation and management.
Clinical Relevance
You may wonder what your anticardiolipin antibodies testing result means for your health. A positive result does not always confirm a diagnosis of antiphospholipid syndrome (APS), especially if you do not have symptoms. The presence of anticardiolipin antibodies alone in asymptomatic individuals does not guarantee clinical outcomes. Your clinical risk depends on several factors, including other risk factors for thrombosis such as smoking, hypertension, thrombocytopenia, and triple APL antibody positivity.
| Evidence Type | Findings |
|---|---|
| Antiphospholipid Antibodies | Presence alone in asymptomatic individuals does not confirm APS or guarantee clinical outcomes. |
| Risk Factors | Independent risk factors for thrombosis include smoking, hypertension, thrombocytopenia, and triple APL antibody positivity. |
| Testing Recommendation | Testing for APL antibodies may be prudent in asymptomatic patients with unexplained prolonged aPTT. |
You should know that false-positive results can occur. These may happen due to infections, medications, or technical issues in the laboratory. Your doctor will consider your clinical history, symptoms, and other laboratory findings before making a diagnosis. Repeat testing helps reduce the chance of false positive results and improves the accuracy of your clinical interpretation.
Next Steps
If your anticardiolipin antibodies testing result is positive, your doctor will look for clinical signs of APS. The diagnostic criteria for APS require both clinical and laboratory evidence. You must have a positive test for lupus anticoagulant (LA), anticardiolipin antibodies, or anti-β2GP1 antibodies on two occasions at least 12 weeks apart. Medium or high titers (>40 GPL or MPL units or >99th percentile) are needed for diagnosis. Your doctor will also check for clinical events such as blood clots or pregnancy complications.
| Criteria | Description |
|---|---|
| Positive for LA or aCL or anti-β2GP1 antibodies | Detected on ≥2 occasions at least 12 weeks apart. |
| aCL antibodies | IgG and/or IgM isotype present in medium or high titer (>40 GPL or MPL units or >99th percentile), measured by standardized ELISA. |
| anti-β2GP1 antibodies | IgG and/or IgM isotype in high titer (>99th percentile), measured by standardized ELISA. |
| Clinical and laboratory criteria | At least 1 clinical and 1 laboratory criterion must be met within a 5-year period. |
You may need repeat testing to confirm your diagnosis. Fluctuating levels of anticardiolipin antibodies can make clinical decisions more difficult. Intermittent positivity complicates the duration of anticoagulation therapy. There are no established guidelines for stopping anticoagulation in patients with changing antibody levels. Your doctor will use caution and consider your clinical history, risk factors, and diagnostic criteria before making recommendations.
- Fluctuating anticardiolipin antibodies levels complicate clinical assessment of thrombotic risk.
- Variability in antibody levels makes management of anticoagulation therapy challenging.
- Your doctor may recommend ongoing monitoring and repeat testing to guide your clinical care.
Tip: Always discuss your anticardiolipin antibodies testing results and interpretation with your healthcare provider. Your doctor will use your clinical history, laboratory findings, and diagnostic criteria to make the best decisions for your health.
Cardiolipin Antibody and Health Risks
Antiphospholipid Syndrome
You may hear your doctor talk about antiphospholipid syndrome when discussing cardiolipin antibody testing. This syndrome is a clinical disorder that happens when your immune system makes antiphospholipid antibodies. These antibodies can increase your risk for thrombosis. You may develop blood clots in your veins, arteries, or small blood vessels. Doctors call these events thrombotic events. You may also face pregnancy morbidity, such as recurrent miscarriages or premature births.
| Clinical Manifestation | Description |
|---|---|
| Thrombotic events | Recurring venous, arterial, and/or microcirculation thrombotic events (e.g., DVTs, stroke, TIAs) |
| Obstetrical complications | Recurrent miscarriages, premature births |
Doctors use clinical criteria to diagnose antiphospholipid syndrome. You need both laboratory evidence of antibody positivity and clinical signs, such as thrombosis or pregnancy morbidity. You may have lupus anticoagulants, anticardiolipin antibodies, or anti-beta2 glycoprotein I antibodies. These antibodies can stay in your blood and raise your risk for future clinical events. If you have antiphospholipid antibodies, your doctor will watch for signs of thrombosis and pregnancy complications.
If you have a history of blood clots or pregnancy loss, ask your doctor about antiphospholipid syndrome. Early detection can help lower your risk for serious clinical problems.
Lupus and Other Conditions
You may wonder how cardiolipin antibodies relate to other diseases. Doctors often find these antibodies in patients with systemic lupus erythematosus. Studies show that 42.4% of patients with lupus test positive for anticardiolipin antibodies. In another study, 25% of lupus patients had these antibodies. You may also have lupus anticoagulants, which can increase your risk for thrombosis.
- 42.4% of patients with systemic lupus erythematosus (SLE) tested positive for anticardiolipin antibodies.
- 25% of a group of 60 lupus patients had anticardiolipin antibodies.
You may also see raised antiphospholipid antibodies in other clinical conditions. These include primary antiphospholipid syndrome, Lyme disease, systemic sclerosis, and Behçet’s syndrome. Doctors use antibody positivity to help diagnose these diseases and assess your risk for thrombosis.
| Condition | Description |
|---|---|
| Systemic Lupus Erythematosus | Commonly associated with raised anticardiolipin antibodies. |
| Primary Antiphospholipid Syndrome | Features raised anticardiolipin antibodies without other defined diseases. |
| Lyme Disease | Anticardiolipin antibodies reported in patients. |
| Systemic Sclerosis | Observed in patients with this condition. |
| Behçet’s Syndrome | Anticardiolipin antibodies reported in this syndrome. |
Doctors look for lupus anticoagulants and other antiphospholipid antibodies when you have unexplained clinical symptoms. These antibodies can increase your risk for thrombosis and other clinical complications.
Pregnancy and Clotting
If you are pregnant or planning to become pregnant, you should know about the clinical risks linked to cardiolipin antibodies. Women with positive cardiolipin antibodies face a higher risk for pregnancy morbidity. You may experience recurrent pregnancy loss or other obstetric problems related to antiphospholipid syndrome. Doctors pay close attention to antibody positivity and lupus anticoagulants during pregnancy.
- Women with positive cardiolipin antibodies are at risk for pregnancy complications.
- Complications include recurrent pregnancy loss and other obstetric morbidities associated with antiphospholipid syndrome.
- The persistence of anticardiolipin antibodies is a significant risk factor for these complications.
You may wonder how these antibodies affect pregnancy. Anticardiolipin antibodies can cause thrombosis in placental vessels. This can lead to placental insufficiency and fetal death. These antibodies may also slow the growth of cells needed for implantation, which can cause miscarriage.
| Study Group | ACA Positive | Control Group | ACA Positive | Live Birth Rate (Study Group) | Live Birth Rate (Control Group) |
|---|---|---|---|---|---|
| Patients | 8 (16%) | 1 (2%) | 49 (98%) | 34 (68%) | 50 (100%) |
In one study, 17.3% of women with recurrent pregnancy loss tested positive for anticardiolipin antibodies. Only 4% of women in the control group had these antibodies. You can see that antibody positivity increases your risk for pregnancy morbidity and lowers your chance of a live birth.
If you have a history of miscarriage or pregnancy complications, talk to your doctor about antiphospholipid antibodies and lupus anticoagulants. Early testing and treatment can help reduce your clinical risk.
Monitoring and Treatment
Repeat Testing
You may need repeat testing for antiphospholipid antibodies if your initial results are positive. Doctors recommend waiting at least 12 weeks before retesting. This helps confirm whether the antibodies are persistent or just temporary. Transient antiphospholipid antibodies can appear after infections or other short-term conditions. Persistent antibodies increase your risk for thrombosis. You should know that test results can change over time. Variability often comes from differences in laboratory methods and the type of assay used. Even the same test can give different results on separate occasions. The presence of antibodies against β2 glycoprotein I can also affect your results. These factors make it important for your doctor to use standardized testing and repeat tests when needed.
- Repeat testing after 12 weeks is recommended for positive results.
- Transient antibodies may disappear over time.
- Persistent antibodies raise your risk for thrombosis.
Treatment Options
If you have persistently positive antiphospholipid antibodies and a history of thrombosis, your doctor may start anticoagulation therapy. You may receive unfractionated or low molecular weight heparin for at least five days. After that, warfarin therapy helps keep your blood clotting levels stable. Doctors aim for an INR between 2 and 3. If you have a high-risk profile or unprovoked thrombosis, lifelong anticoagulation may be necessary. Some patients only need treatment for three to six months. If you have arterial thrombosis or recurrent venous thrombosis, your doctor may recommend high-intensity anticoagulation or combine an antiplatelet agent with low-intensity anticoagulation. Anticoagulant therapies help prevent new blood clots. About 70% of patients respond well to these treatments. Some people do not benefit from standard therapies, so your doctor may adjust your plan. Low-dose aspirin may help some people with antiphospholipid antibodies, but results are mixed.
Lifestyle Impact
Managing antiphospholipid antibodies and thrombosis risk involves lifestyle changes. You can take steps to lower your risk for blood clots. Doctors may recommend aspirin therapy if you have antiphospholipid antibodies but no history of thrombosis. If you have had a blood clot, anticoagulant therapy is necessary. Warfarin therapy requires you to keep your vitamin K intake steady and get regular blood checks. You should avoid smoking, oral contraceptives, and hormone replacement therapy. These factors can increase your risk for thrombosis. If you are pregnant and have recurrent miscarriages, your doctor may suggest low molecular weight heparin as an alternative blood thinner.
| Recommendation | Description |
|---|---|
| Aspirin therapy | Recommended for asymptomatic individuals with antiphospholipid antibodies. |
| Anticoagulant therapy | Necessary for patients with antiphospholipid syndrome who have had a blood clot. |
| Diet considerations with warfarin | Requires stable intake of vitamin K and regular blood checks. |
| Minimize blood clot risk factors | Avoid smoking, oral contraceptives, and hormone replacement therapy. |
| Alternative blood thinners for pregnancy | Low molecular weight heparin may be needed for patients with recurrent miscarriages during pregnancy. |
Long-term monitoring improves your chances of catching problems early. Patients with antiphospholipid antibodies have a higher risk for thrombosis, miscarriages, and lower survival rates. Regular checkups help your doctor adjust your treatment and keep you healthy.
| Outcome | Association with aPL Seropositivity |
|---|---|
| Long-term patient survival | Inferior |
| Renal survival | Inferior |
| Thrombotic events | Higher incidence |
| Miscarriages | Higher incidence |
Tip: Stay in close contact with your healthcare team. Regular monitoring and healthy habits help you manage your risk for thrombosis and improve your quality of life.
Understanding cardiolipin antibody testing helps you take charge of your health.
- The test checks for antibodies that can cause blood clots or pregnancy problems.
- High levels often appear in autoimmune diseases and may need follow-up.
- Early detection and treatment, like anticoagulants or aspirin, lower your risk for serious issues.
- You can find more information from trusted sources such as The Lupus Foundation of America and APS Foundation of America.
Stay proactive and talk with your healthcare provider to keep your health on track.
FAQ
What does a positive cardiolipin antibody test mean?
A positive test shows you have antibodies that may increase your risk for blood clots. You may need repeat testing after 12 weeks. Your doctor will check for symptoms and other risk factors before making a diagnosis.
Can you have cardiolipin antibodies without having a disease?
Yes, you can have these antibodies without any disease. Some people test positive after infections or due to medications. Your doctor looks for symptoms and repeats tests to confirm if you need treatment.
How often should you repeat cardiolipin antibody testing?
Doctors recommend repeat testing at least 12 weeks after your first positive result. This helps confirm if the antibodies are persistent. Persistent antibodies raise your risk for blood clots.
What lifestyle changes help lower your clotting risk?
You can lower your risk by quitting smoking, staying active, and eating a balanced diet. Avoid oral contraceptives and hormone therapy if you have antibodies. Your doctor may suggest aspirin or anticoagulants.
Are cardiolipin antibodies dangerous during pregnancy?
Yes, these antibodies can cause pregnancy problems like miscarriage or premature birth. Your doctor may recommend blood thinners such as low molecular weight heparin. Early testing and treatment improve your chances for a healthy pregnancy.

