News & Events
Comparing Methods for Detecting dsDNA Antibodies in Lupus Patients

You often hear about dsdna antibody testing when doctors discuss lupus. The dsdna antibody serves as a gold standard biomarker for systemic lupus erythematosus (SLE), especially when a clear diagnosis is needed. Most patients with SLE show the presence of the dsdna antibody, with studies reporting rates between 70% and 98%.
- The dsdna antibody appears most frequently in non-Latino Asian, Black, and Latino patients.
It’s important to know that the dsdna antibody helps track lupus nephritis and SLE activity. When dsdna antibody levels rise, your risk for kidney problems increases. The table below shows how the dsdna antibody relates to clinical findings in SLE:
| Evidence Type | Findings | Correlation Strength |
|---|---|---|
| Anti-dsDNA Titer | Elevated in renal flares | Strong positive correlation with SLEDAI |
| C3 and C4 Levels | Low in renal flares | Negative correlation with SLEDAI |
| Non-Renal Flares | Anti-dsdna elevated in 35% | No significant correlation with SLEDAI |
| Remission | Anti-dsdna elevated in 38.5% of renal lupus | N/A |
| Monitoring Frequency | Every 4-6 weeks recommended | N/A |
When searching for the best clinical method to detect the dsdna antibody, you need to consider how each technique impacts diagnosis, monitoring, and prognosis in systemic lupus erythematosus.
Key Takeaways
- Anti-dsDNA antibodies are crucial for diagnosing systemic lupus erythematosus (SLE). A positive test can help confirm the disease and guide treatment.
- Regular monitoring of anti-dsDNA antibody levels is essential. Testing every 4-6 weeks helps track disease activity and predict potential flares.
- Different testing methods exist for detecting anti-dsDNA antibodies. Indirect immunofluorescence offers high specificity, while ELISA provides good sensitivity for routine checks.
- Combining tests can improve accuracy. Your doctor may use multiple methods to ensure reliable results and better manage your lupus care.
dsDNA Antibody Testing in Lupus

Role in Diagnosis
When you visit your doctor with clinical suspicion of SLE, testing for anti-dsdna antibodies becomes a key step. The 2019 EULAR/ACR classification criteria for SLE highlight the importance of anti-dsdna antibodies in diagnosis. These guidelines require that the assays used for anti-dsdna abs must reach at least 90% specificity. This high specificity helps you avoid false positives and ensures that your diagnosis is accurate. The guidelines also give anti-dsdna antibodies the highest score among autoantibodies in the classification criteria for SLE. If you test positive for anti-dsdna abs, you earn 6 out of the 10 points needed for SLE diagnosis. Your doctor may use tests like the Crithidia luciliae immunofluorescence test or the FARR assay because they offer high specificity for anti-dsdna autoantibodies. These tests help confirm systemic lupus erythematosus and guide your treatment plan.
Note: Not all commercial assays for anti-dsdna abs meet the strict specificity required by the classification criteria for SLE. You should ask your healthcare provider which test they use.
Testing for anti-dsdna antibodies also helps your doctor distinguish lupus from other autoimmune diseases. Anti-dsdna abs are rarely found in conditions outside SLE, so their presence supports the diagnosis. You may see anti-dsdna autoantibodies in lupus nephritis, which is a serious manifestation of SLE. The detection of anti-dsdna abs can help your doctor identify systemic manifestations and guide further clinical evaluation.
Role in Monitoring
After your diagnosis, monitoring anti-dsdna antibodies becomes essential for managing SLE. You need regular testing for anti-dsdna antibodies to track disease activity and predict flares. Rheumatology associations recommend that you monitor anti-dsdna abs every 4-6 weeks, especially if you have lupus nephritis or other severe manifestations. Both the absolute value and changes in anti-dsdna titres can signal a flare or remission. If your anti-dsdna abs levels rise, your risk for kidney involvement increases. Your doctor uses these results to adjust your treatment and prevent complications.
- Monitoring anti-dsdna antibodies helps you and your doctor:
- Detect early signs of lupus nephritis
- Assess systemic manifestations
- Guide clinical decisions for medication changes
Testing for anti-dsdna antibodies is not just for diagnosis. It plays a vital role in ongoing clinical care, helping you manage systemic lupus erythematosus and its many manifestations.
Main Anti-dsDNA Detection Methods
When you need to detect anti-dsdna antibodies in SLE, you have several laboratory methods to choose from. Each method offers unique strengths and plays a different role in clinical care. Your doctor selects the most suitable assay based on your symptoms, the need for accuracy, and the resources available in the clinical laboratory. Understanding these methods helps you appreciate how your diagnosis and monitoring are guided.
Indirect Immunofluorescence
Indirect immunofluorescence (IIF) is a classic method for detecting anti-dsdna antibodies. You may hear your doctor mention the Crithidia luciliae immunofluorescence test (CLIFT), which uses a special organism to highlight the presence of anti-dsdna abs. This method stands out for its high specificity, making it valuable for confirming systemic lupus erythematosus.
- IIF is often used together with enzyme-linked immunosorbent assay (ELISA) to provide a complete picture of your autoantibody profile.
- The combination of IIF and ELISA increases the positive predictive value for SLE diagnosis and flare detection.
- IIF is especially helpful when your doctor needs to rule out false positives and confirm anti-dsdna abs in complex cases.
You can see how IIF compares to other methods in the table below:
| Detection Method | Sensitivity (%) | Specificity (%) | Correlation with SLEDAI | Renal Involvement Differentiation |
|---|---|---|---|---|
| IIF | 38.92 | 98.31 | – | p < 0.05 |
| CLIA | 41.57 | – | R = 0.29, p = 0.015 | p < 0.001 |
| DLCM | – | – | R = 0.42, p < 0.001 | p = 0.132 |
| Combined Assays | 56.64 (IIF+DLCM) | 53.73 | – | – |
IIF provides high specificity, which means you can trust a positive result for anti-dsdna antibodies. However, sensitivity varies across studies. Some report sensitivity as high as 95.7%, while others show lower rates. Your doctor may choose IIF when accuracy is critical for your diagnosis.
ELISA for Anti-dsDNA
ELISA (enzyme-linked immunosorbent assay) is a popular choice for screening anti-dsdna antibodies. You benefit from ELISA’s high sensitivity, which helps detect even low levels of anti-dsdna abs. This method is simple, cost-effective, and provides quantitative results that help your doctor monitor your disease over time.
- ELISA is easy to perform and does not require advanced technical skills.
- You get measurable concentrations of anti-dsdna antibodies, which guide your treatment and track SLE activity.
- ELISA is widely available in clinical laboratories, making it accessible for routine monitoring.
Here are some advantages of ELISA for anti-dsdna detection:
| Advantage | Description |
|---|---|
| High Sensitivity | ELISA can detect low levels of anti-dsdna antibodies. |
| Quantitative Results | You receive exact numbers for antibody levels, useful for monitoring. |
| Simplicity | The test is straightforward and easy to perform. |
| Cost-Effectiveness | ELISA is less expensive than many other assays. |
ELISA’s sensitivity for SLE patients reaches 77.3%, but specificity is lower at 42.4%. This means ELISA is great for initial screening, but your doctor may use another method to confirm a positive result.
Chemiluminescent Immunoassay
Chemiluminescent immunoassay (CLIA) is a modern technique for detecting anti-dsdna antibodies. You benefit from CLIA’s high sensitivity and automation, which make it ideal for busy clinical settings. CLIA uses light emission to measure antibody levels, providing fast and accurate results.
- CLIA offers 100% sensitivity and 82% specificity for anti-dsdna detection.
- The method works quickly, often delivering results in 30–40 minutes.
- Automation ensures consistent quality and reduces errors in the clinical laboratory.
You can see how CLIA compares to other assays in the chart below:
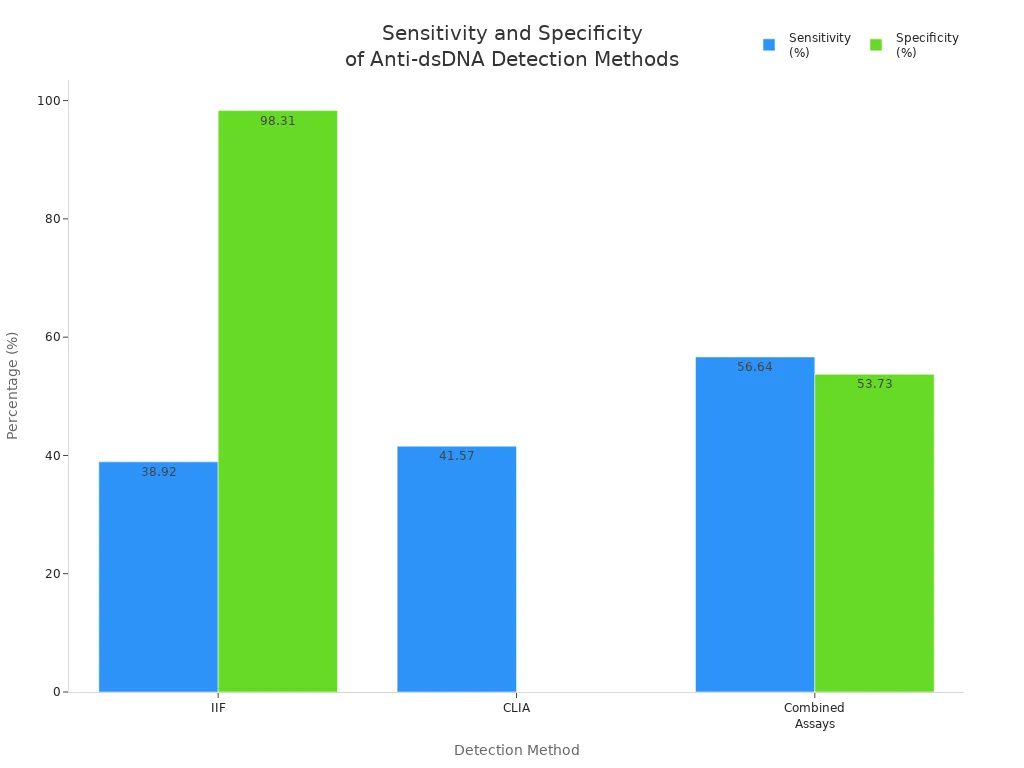
CLIA’s wide dynamic range allows your doctor to detect elevated anti-dsdna abs without diluting your sample. This method is especially useful for early prediction of autoimmune diseases and reduces the need for invasive procedures.
Digital Liquid Chip
Digital liquid chip method (DLCM) is a new technology for detecting anti-dsdna antibodies. You benefit from DLCM’s ability to test for multiple autoantibodies at once, using barcoded magnetic beads. This high-throughput approach is valuable for systemic lupus erythematosus, where many autoantibodies may be present.
- DLCM allows simultaneous detection of several autoantibodies in a single sample.
- The method increases efficiency and throughput in clinical laboratories.
- DLCM shows a strong correlation with SLEDAI scores, helping your doctor track disease activity.
The table below highlights DLCM’s performance:
| Assay Type | Sensitivity (%) | Specificity (%) | AUC |
|---|---|---|---|
| DLCM | 86.87 | N/A | 0.938 |
| CLIA | N/A | 94.03 | N/A |
DLCM is especially useful when your doctor needs a comprehensive autoimmune profile. This method supports accurate monitoring and helps differentiate between SLE and other autoimmune diseases.
Tip: Your doctor may combine different assays to improve sensitivity for lupus nephritis detection. However, combining tests can reduce specificity, so your doctor balances these factors based on your clinical needs.
Choosing the right method for anti-dsdna antibody detection is crucial for accurate diagnosis and monitoring in SLE. Each assay offers unique benefits, and your doctor selects the best option based on your symptoms, disease activity, and laboratory resources.
Indirect Immunofluorescence for Anti-Double Stranded DNA Antibodies
How It Works
You may wonder how indirect immunofluorescence helps your doctor detect anti-dsdna antibodies in SLE. This method uses a special slide with the Crithidia luciliae organism. The organism contains a unique structure called a kinetoplast, which holds pure double stranded DNA. When your blood sample is added, any anti-dsdna abs will bind to the DNA in the kinetoplast. A fluorescent dye attaches to these antibodies. Under a microscope, you see a bright signal if anti-dsdna abs are present. This process gives you a clear answer about the presence of anti-dsdna antibodies in your sample.
Strengths
Indirect immunofluorescence stands out for its high specificity in detecting anti-dsdna abs. You get reliable results that help confirm SLE, especially when other assays show unclear findings. Doctors trust this method for its ability to reduce false positives. The positive predictive value is also very high, which means a positive result strongly suggests SLE. You can see the strengths of this method in the table below:
| Assay Type | Specificity (%) | Positive Predictive Value (%) | Sensitivity (%) |
|---|---|---|---|
| IIF | 98.31 | 96.10 | 38.92 |
| CLIA | N/A | N/A | 41.57 |
| DLCM | N/A | N/A | 43.65 |
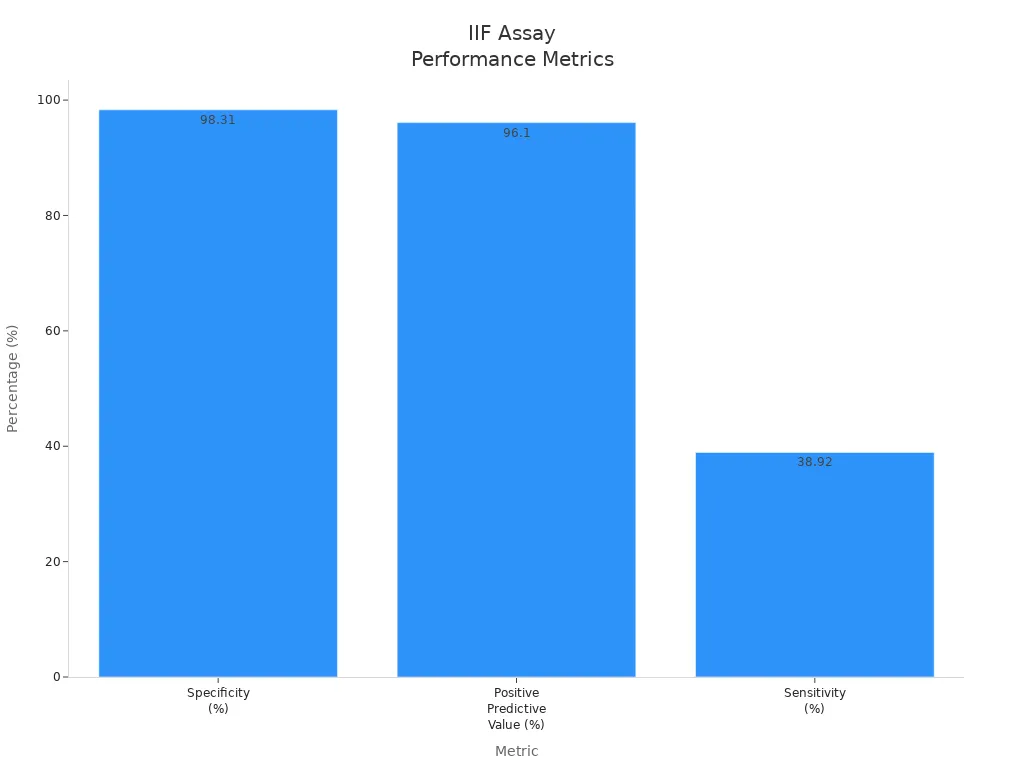
You benefit from this high specificity when your doctor needs to confirm SLE or lupus erythematosus. Indirect immunofluorescence is especially useful for detecting autoantibodies to dsdna in clinical settings where accuracy matters most.
Limitations
You should know that indirect immunofluorescence has some limitations. The sensitivity is lower than other assays, so you may not detect all cases of anti-dsdna abs. If you have low levels of anti-dsdna antibodies, this method might miss them. The test requires skilled laboratory staff and special equipment. You may wait longer for results compared to automated assays. Sometimes, clinical labs use indirect immunofluorescence together with ELISA or chemiluminescent immunoassay to improve detection of anti-dsdna abs. This combination helps balance sensitivity and specificity for SLE diagnosis and monitoring. You may need more than one test to get a complete picture of your autoimmune status.
ELISA for Anti-dsDNA Antibodies

How It Works
You may see ELISA used often in clinical labs to detect anti-dsdna antibodies in patients with SLE. This method uses a step-by-step process to measure anti-dsdna abs in your blood. Here is how the ELISA assay works for anti-dsdna detection:
- Coat microtiter plates with a small amount of ultrapure nucleosome preparation in sodium carbonate buffer for several hours at a cold temperature.
- Add a layer of highly purified, native dsDNA in the same buffer and let it sit overnight.
- Wash the plates with a gentle solution to remove unbound material.
- Block the plates with a protein solution to prevent non-specific binding.
- Add your diluted serum and let it react for half an hour.
- Use a special enzyme-linked antibody to detect any bound anti-dsdna abs.
- Add a color-changing chemical and wait for the reaction.
- Measure the color intensity using a spectrophotometer.
- Create a standard curve using known positive samples.
- Calculate the amount of anti-dsdna antibodies in your sample and set the cutoff for positive results.
This process helps your doctor get accurate and quantitative results for anti-dsdna abs. You can trust ELISA assays to provide clear numbers for clinical decision-making.
Strengths
ELISA offers several strengths for detecting anti-dsdna antibodies in SLE. You benefit from its ability to serve as a serological marker for diagnosis and disease activity. ELISA assays can measure both single-stranded and double-stranded DNA antibodies, which helps your doctor understand your autoimmune status. The table below shows some important strengths and challenges:
| Strengths of ELISA for anti-dsdna detection | Challenges in detection |
|---|---|
| Utility as serological markers for SLE diagnosis and disease activity assessment | Methodological heterogeneity in detection |
| Combining with other biomarkers enhances diagnostic sensitivity | Need for more reliable biomarkers for diagnosis and stratification |
You may notice that ELISA assays work well when combined with other clinical tests. This combination increases sensitivity and helps your doctor make better decisions about your systemic erythematosus care. ELISA also provides quantitative results, making it easier to monitor changes in anti-dsdna abs over time.
ELISA assays play a key role in tracking anti-dsdna antibodies during SLE flares and remission. You can rely on these tests for regular clinical monitoring.
Limitations
You should know that ELISA assays have some limitations in clinical practice. Different ELISA tests may use various antigens, which leads to poor consistency between results. This inconsistency makes it hard for your doctor to compare anti-dsdna abs levels across different labs. The table below highlights some main limitations:
| Limitation | Description |
|---|---|
| Poor consistency between methodologies | Different affinities of antigens and antibodies complicate clinical use. |
| Variability in sensitivity and specificity | Sensitivity and specificity can change depending on the assay used. |
| Inconsistency between different ELISA tests | Not all ELISA tests are comparable due to varying antigen avidities. |
| Detection of different subpopulations | Some assays detect different anti-dsdna subpopulations, which may confuse clinical significance. |
You may find that ELISA assays sometimes detect anti-dsdna abs that do not match your clinical symptoms. Your doctor may need to use other assays to confirm results and guide your treatment for systemic lupus erythematosus. ELISA remains a valuable tool, but you should understand its limitations in clinical settings.
Chemiluminescent Immunoassay for dsDNA Antibody
How It Works
You may see chemiluminescent immunoassay used in many clinical labs to detect anti-dsdna antibodies in patients with sle. This method uses a special chemical reaction that produces light. When you add your blood sample to the test, anti-dsdna abs bind to dsDNA coated on beads or plates. The assay then adds a reagent that reacts with these antibodies and emits light. Machines measure the brightness of the light to determine how much anti-dsdna is present. You get results quickly, often within an hour. This process helps your doctor track sle activity and monitor anti-dsdna abs during treatment.
Strengths
Chemiluminescent immunoassay offers several strengths for anti-dsdna detection in sle. You benefit from high sensitivity, which means the test can find even small amounts of anti-dsdna antibodies. The method works well for routine clinical monitoring because it is automated and reduces human error. You get consistent results, which help your doctor make decisions about your systemic erythematosus care. Many clinical labs prefer this assay for its speed and reliability. You can also use chemiluminescent immunoassay to measure changes in anti-dsdna abs over time, which is important for tracking disease flares.
Tip: Automated assays like chemiluminescent immunoassay help labs process many samples at once, making them ideal for busy clinical settings.
Limitations
You should know that chemiluminescent immunoassay has some limitations when detecting anti-dsdna antibodies in sle. Studies show that sensitivity and specificity can vary compared to other assays. You may see different results depending on the brand or type of assay used. Lack of standardization among assays leads to significant variations in clinical performance. Researchers recommend further studies with larger groups to confirm how well these assays work in real-world clinical settings. The table below highlights key limitations:
| Limitation Description | Source |
|---|---|
| Variability in sensitivity and specificity compared to other methods | Clinical Comparison of QUANTA Flash dsDNA Chemiluminescent Immunoassay |
| Lack of standardization among assays confirmed by significant variations | Clinical Comparison of QUANTA Flash dsDNA Chemiluminescent Immunoassay |
| Need for further studies with larger cohorts to confirm clinical performance | Clinical Comparison of QUANTA Flash dsDNA Chemiluminescent Immunoassay |
You may need to combine chemiluminescent immunoassay with other assays to improve accuracy for anti-dsdna abs detection in sle. Your doctor considers these limitations when choosing the best method for your clinical care.
Digital Liquid Chip and Anti-dsDNA Detection
How It Works
You may see digital liquid chip technology used in clinical labs to detect anti-dsdna antibodies in patients with sle. This method uses tiny magnetic beads that carry barcodes. Each bead can capture a different autoantibody, including anti-dsdna abs. When you add your blood sample, anti-dsdna antibodies attach to the beads. The machine reads the barcodes and measures the amount of anti-dsdna present. You get results for many autoantibodies at once. This process helps your doctor understand your autoimmune status and track systemic erythematosus.
Strengths
Digital liquid chip assays offer several strengths for clinical detection of anti-dsdna abs in sle. You benefit from high sensitivity, which means the test finds even small amounts of anti-dsdna antibodies. The method can test for multiple autoantibodies in one sample. You save time and get a complete autoimmune profile. Clinical studies show that digital liquid chip assays have a strong correlation with disease activity scores in sle. You help your doctor make better decisions about your treatment. The table below shows some key strengths:
| Strength | Description |
|---|---|
| High Sensitivity | Detects low levels of anti-dsdna antibodies |
| Multiplex Capability | Tests for many autoantibodies at once |
| Fast Results | Provides quick answers for clinical decisions |
| Strong Correlation | Matches well with sle activity and flares |
Tip: You may see digital liquid chip assays used when your doctor needs to monitor sle and predict flares.
Limitations
You should know that digital liquid chip assays have some limitations in clinical practice. The method may cost more than other anti-dsdna detection assays. Some labs may not have the equipment needed for these tests. You may see differences in results between labs because of technical factors. Clinical experts recommend combining digital liquid chip assays with other methods to confirm anti-dsdna abs in sle. You may need more than one test to get the most accurate results. Sometimes, the test may not detect all anti-dsdna antibodies if your levels are very low. Your doctor considers these factors when choosing the best clinical assay for your care.
Comparing Anti-dsDNA Antibody Detection Methods
Sensitivity and Specificity
You need to know how well each anti-dsdna antibody test works. Sensitivity tells you how often a test finds anti-dsdna abs when you have sle. Specificity shows how often a test gives a true negative when you do not have sle. These two numbers help you and your doctor choose the best test for diagnosis and monitoring.
- Anti-dsdna antibody testing shows big differences in specificity. This can change how your doctor manages sle.
- Some assays, like the anti-dsdna-NcX ELISA, reach high specificity (0.9), while others, like ELiA dsDNA, go even higher (0.959).
- Sensitivity varies more. The anti-dsdna-NcX ELISA has a sensitivity of 0.51, but ELiA dsDNA drops to 0.38.
You see that no single test is perfect. High specificity helps confirm sle, but lower sensitivity means some cases may be missed. Your doctor may use more than one test to get the most accurate results. The sensitivity of hallmark autoantibodies, like anti-dsdna abs, can change depending on the method.
| Assay Name | Sensitivity | Specificity |
|---|---|---|
| anti-dsdna-NcX ELISA | 0.51 | 0.90 |
| ELiA dsDNA | 0.38 | 0.959 |
High specificity means you can trust a positive result. Lower sensitivity means you may need extra tests if your symptoms suggest sle.
Practicality
You want a test that fits your needs and your clinic’s resources. Practicality means looking at cost, speed, and how easy it is to run the test. Most anti-dsdna antibody tests take 2 to 3 days to give results. Some newer assays, like chemiluminescent immunoassay, work faster and use machines to process many samples at once.
- ELISA is simple and cost-effective. Many clinics use it for routine sle monitoring.
- Indirect immunofluorescence needs skilled staff and special slides. It takes longer and costs more.
- Chemiluminescent immunoassay gives quick results and works well in busy labs.
- Digital liquid chip assays test for many autoantibodies at once, but they cost more and need special equipment.
You should ask your doctor which test fits your situation. If you need fast results, chemiluminescent immunoassay may help. If your clinic wants to save money, ELISA is a good choice. Some tests need more training and tools, so not every lab can run them.
Clinical Usefulness
You want a test that helps your doctor make good decisions about your sle care. Clinical usefulness means how well the test helps with diagnosis, monitoring, and predicting lupus nephritis. The predictive value of anti-dsdna antibodies depends on the test and your symptoms.
The clinical use of anti-dsdna antibodies goes beyond diagnosis. You use these tests to track disease activity and guide treatment. Some tests work better for certain tasks:
- Indirect immunofluorescence gives high specificity. You use it to confirm sle when you need a clear answer.
- ELISA helps with regular monitoring. You get numbers that show changes in anti-dsdna abs over time.
- Chemiluminescent immunoassay works well for fast, automated testing. You use it in busy clinics for sle monitoring.
- Digital liquid chip assays help when you need to check many autoantibodies at once. You use them for a full autoimmune profile.
Recent studies show that anti-dsdna IgE is a strong biomarker for predicting lupus nephritis relapse. You may find anti-dsdna IgE more useful than anti-dsdna IgG for monitoring disease activity and guiding treatment. Your doctor can use anti-dsdna IgE with other clinical factors to assess your risk and plan your care.
Tip: You may need more than one test to get the best results. Your doctor combines tests to balance sensitivity and specificity for your sle management.
| Task | Best Assay(s) |
|---|---|
| Confirming Diagnosis | Indirect Immunofluorescence |
| Routine Monitoring | ELISA, Chemiluminescent Immunoassay |
| Predicting Lupus Nephritis | Anti-dsdna IgE, Digital Liquid Chip |
You see that each test has strengths and weaknesses. You and your doctor choose the best assay based on your symptoms, clinic resources, and the need for accuracy. The right test helps you manage systemic lupus erythematosus and improves your outcomes.
Choosing the Best Method for Lupus Care
Initial Diagnosis
When your doctor suspects sle, choosing the right anti-dsdna detection method matters. You start with antinuclear antibody testing, which acts as an entry point for systemic lupus erythematosus diagnosis. Anti-dsdna antibodies play a key role in confirming sle. Experts recommend using solid-phase assays and immunofluorescence tests for initial screening. You may see your doctor use a double-screening strategy. First, you get a last-generation solid-phase assay. If you test positive, your doctor confirms the result with the Farr or Crithidia luciliae immunofluorescence test. This approach increases clinical accuracy and reduces false positives.
Tip: Anti-dsdna abs help your doctor confirm lupus and guide your treatment plan.
Recommended Diagnostic Approach:
- Start with solid-phase assays for anti-dsdna abs.
- Confirm positive results with immunofluorescence tests.
- Use anti-dsdna autoantibodies as a key immunological criterion.
| Recommendation | Description |
|---|---|
| Use of anti-dsdna autoantibodies | Effective indicators for sle diagnosis and treatment response. |
| Testing methods | Solid-phase assays and radioimmunoassay are recommended for anti-dsdna abs. |
| Double-screening strategy | Combine solid-phase assay with immunofluorescence for best clinical results. |
Disease Activity Monitoring
After diagnosis, you need regular monitoring of anti-dsdna antibodies to track sle activity. Anti-dsdna abs show changes in disease status and help your doctor adjust your treatment. You benefit from assays that provide quantitative results, such as ELISA or chemiluminescent immunoassay. These tests allow you to see trends in anti-dsdna levels over time. Your doctor uses these results to predict lupus nephritis and manage systemic symptoms. Clinical guidelines suggest using anti-dsdna abs as effective indicators for monitoring disease activity and treatment response.
- ELISA and chemiluminescent immunoassay work well for routine monitoring.
- You get fast, reliable results that support clinical decisions.
Special Considerations
You may face special situations in lupus care. Some clinical labs use digital liquid chip assays to test for multiple autoantibodies at once. This method helps when you need a full autoimmune profile. If your symptoms are complex, your doctor may combine different assays to improve sensitivity and specificity. You should know that anti-dsdna abs detection can vary between labs. Always ask your doctor which assays they use and how results guide your care. Anti-dsdna antibodies remain central to systemic lupus erythematosus management, especially for monitoring and predicting lupus nephritis.
Note: Combining assays can improve detection but may lower specificity. Your doctor balances these factors for your best clinical outcome.
You see that anti-dsdna antibodies play a key role in sle diagnosis and monitoring. Each clinical assay for anti-dsdna abs has strengths and weaknesses. Indirect immunofluorescence gives high specificity for sle, while ELISA and chemiluminescent immunoassay offer practical options for routine clinical care. Digital liquid chip assays help you check many autoantibodies at once. You should ask your doctor which anti-dsdna abs test fits your clinical needs. Advances in anti-dsdna antibody detection will improve lupus outcomes and support better systemic erythematosus care.
FAQ
What is the most accurate test for anti-dsDNA antibodies?
You get the highest accuracy from the Crithidia luciliae immunofluorescence test. This test shows over 98% specificity. Doctors use it to confirm lupus when other tests give unclear results.
How often should you check anti-dsDNA antibody levels?
You should test every 4 to 6 weeks if you have lupus. Regular checks help your doctor spot flares early and adjust your treatment.
Can you use more than one test for lupus diagnosis?
Yes, you can. Doctors often combine ELISA and immunofluorescence. This approach increases sensitivity and specificity. You get a clearer diagnosis.
Tip: Ask your doctor which tests they use and why. This helps you understand your care plan.
Which method works best for monitoring lupus nephritis?
| Method | Usefulness for Nephritis |
|---|---|
| Anti-dsDNA IgE | High |
| Chemiluminescent Assay | Good |
| ELISA | Moderate |
You get the best prediction for lupus nephritis relapse from anti-dsDNA IgE tests.

