News & Events
Hepatitis C Antibody Testing Made Simple for Primary Care

You play a vital role in detecting hepatitis early in primary care. Early use of the hepatitis c antibody test helps you prevent serious health problems like cirrhosis and liver cancer.
- Early treatment saves lives and lowers costs for patients and clinics.
- People with hepatitis face much higher medical expenses than those without infection.
You can confidently use simple steps to make testing easy and effective for everyone.
Key Takeaways
- Early detection of hepatitis C through antibody testing can save lives and reduce healthcare costs.
- Universal screening is recommended for all adults aged 18 and older, especially for high-risk groups.
- Always confirm a positive antibody test with an HCV RNA test to ensure accurate diagnosis and treatment.
- Use clear communication to help patients understand the importance of testing and follow-up care.
- Integrate hepatitis C testing into routine practice to improve screening rates and patient outcomes.
Hepatitis C Antibody Basics
What Is the Hepatitis C Antibody Test
You use the hepatitis c antibody test to find out if someone has ever been exposed to the hepatitis C virus. This test looks for special proteins, called antibodies, in the blood. Your body makes these antibodies when it tries to fight off the virus. The test uses a method called enzyme immunoassay to detect these antibodies, especially a type called immunoglobulin G (IgG). If you see these antibodies in a patient’s blood, it means their immune system has responded to the virus at some point. However, these antibodies do not protect against future infections or cure the disease.
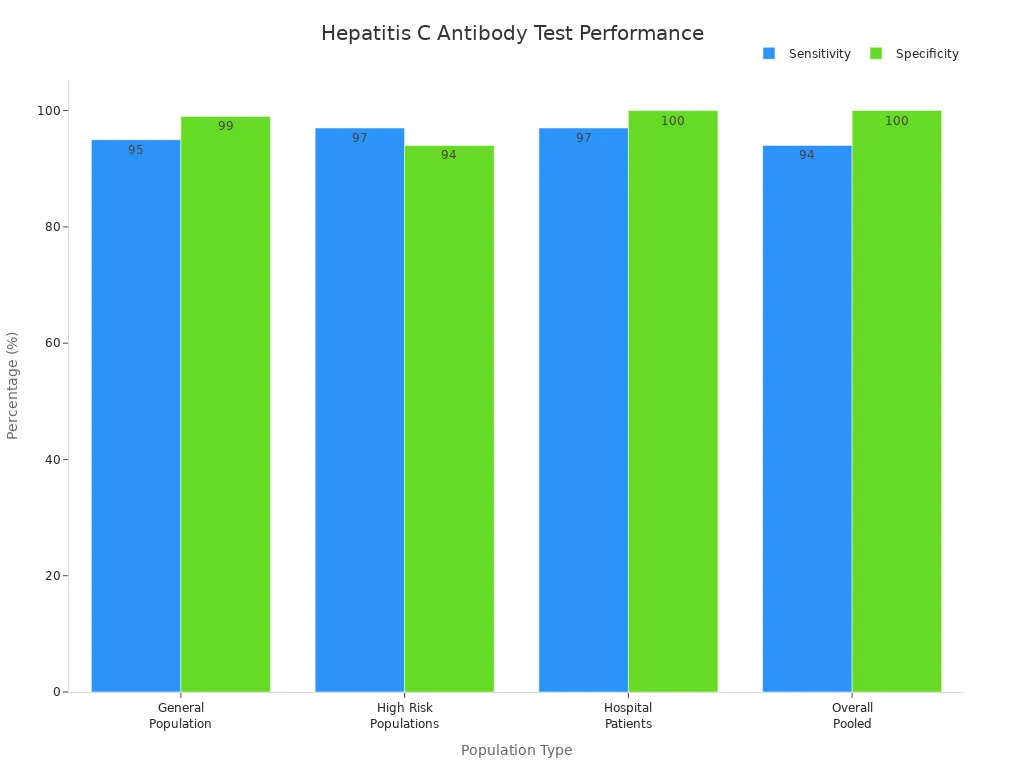
The hepatitis c antibody test works well for most people. You can see how accurate it is in different groups:
| Population Type | Sensitivity (%) | Specificity (%) |
|---|---|---|
| General Population | 95% (95% CI 94%-96%) | 99% (95% CI 98%-99%) |
| High Risk Populations | 97% (95% CI 96%-98%) | 94% (95% CI 94%-95%) |
| Hospital Patients | 97% (95% CI 96%-98%) | 100% (95% CI 100%-100%) |
| Overall (Pooled) | 94% (95% CI 93%-96%) | 100% (95% CI 100%-100%) |
How It Detects Hepatitis C Virus
The hepatitis c antibody test does not look for the virus itself. Instead, it checks for antibodies your immune system makes after infection. These antibodies usually show up in the blood about six months after infection. When you order this test, you are checking if the patient’s immune system has ever seen the hepatitis C virus.
Here is how the process works:
| Evidence Description | Key Points |
|---|---|
| Antibody Detection | The test looks for antibodies to HCV in the blood, indicating past infection. |
| Immune Response | Antibodies are proteins produced by the immune system in response to HCV infection. |
| Current Infection | A positive result does not confirm a current infection; further testing is needed. |
Tip: A positive hepatitis c antibody test means the person has been exposed to the virus, but you need another test to see if the infection is still active.
The hepatitis c antibody test helps you find people who have ever had the virus, even if they do not feel sick. This makes it a powerful tool for early detection and better patient care.
Why Hepatitis Screening Matters
Who Should Be Tested
You help protect your patients by knowing who needs hepatitis testing. The latest guidelines recommend universal screening for all adults 18 years and older at least once in their lifetime, except in areas where hepatitis infection rates are very low. Pregnant women should get tested during each pregnancy. You should also focus on high-risk groups. These include people with HIV, those who have ever injected drugs, and anyone with certain medical conditions. Children born to mothers with hepatitis infection need testing too.
Here is a quick guide to current recommendations:
| Screening Recommendation | Details |
|---|---|
| Universal Screening | All adults 18+ at least once, except in very low prevalence areas |
| Pregnant Women | Test during each pregnancy |
| High-Risk Groups | One-time testing for those with risk factors |
| Routine Testing | Periodic testing for ongoing risk |
| Testing Protocol | Start with antibody test, follow with RNA if positive |
You should pay special attention to these high-risk populations:
- Persons with HIV
- Persons who ever injected drugs and shared needles
- Persons with selected medical conditions, such as those on hemodialysis
- Prior recipients of transfusions or organ transplants before certain dates
- Health care and public safety workers exposed to hepatitis infection
- Children born to mothers with hepatitis infection
Benefits of Early Detection
You make a big difference when you find hepatitis infection early. Early diagnosis lets patients start treatment before liver damage occurs. You help patients learn how to prevent spreading the infection to others. Modern antiviral medicines work best when you begin treatment early. Nearly one-third of people with hepatitis infection do not know they have it. This lack of awareness can lead to accidental transmission.
Note: Timely diagnosis is the first step in a complete care plan. When you link patients to treatment quickly, you give them access to therapies that can cure hepatitis infection and lower the risk of spreading the virus.
Early detection saves lives, reduces health care costs, and improves outcomes for your patients. You help stop the spread of hepatitis infection in your community.
Diagnostic Tests for Hepatitis C

Antibody vs. RNA Tests
You start hepatitis C screening with an antibody test. This test helps you find out if your patient has ever been exposed to the virus. If the antibody test comes back positive, you need to order an RNA test next. The RNA test looks for the actual virus in the blood. It tells you if the infection is active right now.
Here is a simple comparison of the two main diagnostic tests:
| Test Type | Diagnostic Accuracy | Distinction of Infection Type |
|---|---|---|
| Antibody Tests | High sensitivity and specificity for screening | Cannot distinguish between current and resolved infections |
| RNA Tests | Directly detect the presence of the virus | Essential for confirming active infections |
You use antibody tests for initial screening. You rely on RNA tests to confirm active hepatitis C infection. This two-step process helps you make the right diagnosis and guide treatment.
Window Period and Limitations
You need to know about the window period when using hepatitis C diagnostic tests. The window period is the time after someone gets infected but before antibodies show up in the blood. This period usually lasts from 45 to 68 days. If you test too early, the antibody test may not find the infection.
Here are some important limitations to remember:
- The window period can cause false-negative results because antibodies have not developed yet.
- Immunocompromised patients may not produce enough antibodies, which can lead to misdiagnosis.
- Testing during the window period may miss early infections.
Tip: If you suspect recent exposure, consider repeating the antibody test after the window period or use an RNA test for earlier detection.
You improve diagnostic accuracy by understanding these limitations. You help your patients get the right care at the right time.
Ordering Hepatitis C Antibody Tests
Step-by-Step Guide
You can order hepatitis C antibody tests in your clinic with a clear process. These steps help you follow clinical guidelines and make sure your patients get the right care. Use this guide to keep your workflow simple and effective:
- Start with a laboratory-based or point-of-care rapid antibody test for hepatitis C.
- If the antibody test is positive, order an HCV RNA test to check for active infection.
- If the antibody test is negative but you suspect recent infection, order an HCV RNA test to rule out early cases.
- For patients with a history of a positive antibody test, use an HCV RNA test for current screening.
- After a known exposure, order a baseline antibody test. If positive, follow up with an HCV RNA test and liver function tests.
- If the HCV RNA test is positive after a positive antibody test, refer the patient for treatment evaluation.
Tip: Always confirm active infection with an HCV RNA test after a positive antibody test. This step ensures you do not miss ongoing infections.
You can use these steps for all patients who need hepatitis C screening. These tests help you find both past and current infections.
Choosing the Right Patients
You need to know which patients should get hepatitis C antibody tests. Clinical guidelines make this choice easier. You should offer tests to:
- All adults aged 18 and older at least once in their lifetime
- Pregnant individuals during each pregnancy
- Anyone with risk factors, such as:
- People with HIV
- Individuals who have ever injected drugs and shared equipment
- Those on maintenance hemodialysis or with abnormal liver tests
- Recipients of transfusions or organ transplants before safety screening dates
- Health care workers after exposure to infected blood
- Children born to mothers with hepatitis C
- Anyone with ongoing risk factors should get routine periodic tests
- Anyone who requests testing, even without risk disclosure
These criteria help you reach more patients who may benefit from early detection. You make a difference by using tests to find infections before symptoms appear.
Interpreting Diagnostic Results
Negative, Positive, and Indeterminate
You need to understand how to interpret hepatitis C antibody test results. Each result gives you important clues about your patient’s health. You see three main types of results: negative, positive, and indeterminate.
- A negative antibody result means your patient has not been exposed to the hepatitis C virus. You do not need to order more tests if you see this result, unless you suspect recent exposure during the window period.
- A positive antibody result can mean several things. Your patient may have a current, active hepatitis C infection. Sometimes, a positive result shows a past infection that has already cleared. In some cases, the test gives a false positive result. Studies show that false positives can happen in up to 22% of cases, especially in low-risk populations.
- An indeterminate antibody result means the test did not clearly show if your patient has hepatitis C antibodies. This can happen because of a non-specific reaction or a very early infection. Sometimes, indeterminate results are false positives. Other times, they suggest a real infection that is just starting.
Here is a table to help you with interpretation:
| Result Type | Interpretation |
|---|---|
| Negative | No evidence of hepatitis C exposure |
| Positive | Current, active infection; prior resolved infection (20%-37% of cases); false positive possible |
| Indeterminate | Non-specific reaction (false positive); possible early or pre-existing infection |
You see that antibody results do not always give you a clear answer. You need to look at the full picture before making decisions.
Tip: Always confirm a positive antibody result with an RNA test. This step helps you avoid mistakes and gives your patient the best care.
Next Steps After Each Result
You must know what to do after you get each type of antibody test result. Your actions help your patients get the right diagnosis and treatment.
| Test Result | Next Step |
|---|---|
| HCV antibody-negative | No further action needed; no viral load test required. |
| HCV antibody-positive | Order an HCV RNA test to confirm active infection. |
| HCV antibody-positive, viral load-negative | Patient has cleared the virus; no treatment needed. |
| HCV antibody-positive, viral load-positive | Patient has active hepatitis C; start treatment process. |
| Indeterminate antibody result | Repeat the antibody test or order an HCV RNA test. |
You use the RNA test as the gold standard for confirming active hepatitis C infection. This test finds the virus in the blood and measures the viral load. You rely on RNA testing because it gives you accurate information about the presence of the virus. It also helps you decide if your patient needs treatment and lets you track how well therapy works.
Follow these steps to manage your patients:
- If you see a negative antibody result, reassure your patient. No further testing is needed unless you suspect recent exposure.
- If you see a positive antibody result, order an RNA test. This confirms if the infection is active.
- If the RNA test is negative after a positive antibody result, tell your patient they have cleared the virus.
- If the RNA test is positive, start the treatment process and refer your patient to a specialist.
- If you see an indeterminate antibody result, repeat the test or use an RNA test to clarify the diagnosis.
Note: You improve patient outcomes by following these steps. You help your patients understand their results and guide them toward the right care.
You make a big difference by interpreting antibody results correctly. You use RNA testing to confirm active infection and avoid unnecessary treatments. You help your patients get the answers they need.
Clinical Significance for Primary Care
Confirmatory Testing
You play a key role in confirming hepatitis C infection. When you interpret test results correctly, you guide your patients toward the right care. You start with the antibody test. If the result is reactive, you order an HCV RNA test to check for active infection. This step helps you avoid unnecessary treatment and ensures that only patients with current infection receive therapy.
Here is a simple table to help you understand what each result means and what you should do next:
| Test Result | Interpretation | Next Steps |
|---|---|---|
| Non-reactive | No exposure to HCV | No further action needed |
| Reactive | Potential exposure | Order HCV RNA test |
| HCV RNA detected | Active infection | Initiate treatment |
| HCV RNA not detected | Past infection or false positive | Monitor and reassess |
Tip: Always confirm a reactive antibody result with an HCV RNA test. This step helps you identify patients who need treatment and those who do not.
Patient Management
You help patients manage hepatitis C by following best practices. You work with specialty pharmacies to make sure patients get their medicine quickly. You support patients through phone calls or telemedicine visits to keep them on track with treatment. You teach patients to request refills at least one week before they run out of medicine. You connect patients with community health workers or navigators who help them stay in care after diagnosis.
- Partner with specialty pharmacies to speed up medication approval.
- Provide support through phone or telemedicine visits.
- Remind patients to request refills early.
- Use community health workers to help patients stay in care.
- Treat all patients with chronic hepatitis C if they have a life expectancy of at least one year.
- Order extra lab tests for patients with advanced liver disease or other health problems.
You see that treatment rates have improved over time. In one study, less than 10% of patients started treatment within two years. A newer study showed that over 40% began treatment, with an average wait of 33 days. Patients with commercial insurance were more likely to get treatment than those with Medicaid.
Note: You can help more patients start treatment by removing barriers and supporting them throughout the process. Your actions improve health outcomes and reduce the spread of hepatitis C in your community.
Common Pitfalls
Misinterpretation
You may face challenges when interpreting hepatitis C antibody test results. Many providers make mistakes by relying only on a positive screening test. You should not conclude that a patient has hepatitis C infection based on this result alone. Always confirm with a supplemental test that has high specificity. If you skip this step, you risk confusing indeterminate results or missing the chance to spot a false positive. Some tests can show a false result, especially in low-risk patients. This can lead to extra anxiety and unnecessary medical costs. You might also order screening tests incorrectly because of clerical mistakes or unfamiliarity with guidelines. These errors can cause false positives and negatives, making it harder to give the right care.
Tip: Always use a two-step process. Confirm every positive antibody test with an RNA test to avoid acting on a false result.
Missed Follow-Up
You need to pay close attention to follow-up after a positive hepatitis C antibody test. Many patients do not return for further care. Loss to follow-up means patients miss the chance to cure their infection. Untreated hepatitis C can lead to serious health problems. You see many patients lost at different stages of care. This increases the number of untreated infections and raises the risk of liver disease. Missed follow-up also means more people live with hepatitis C without knowing it. You help prevent this by tracking patients and making sure they complete every step.
- Patients lost to follow-up do not get the care they need.
- Untreated infections increase illness and health costs.
- You can reduce missed follow-up by using reminders and patient navigators.
Note: Careful follow-up helps you cure more patients and lower the risk of complications.
Practical Tips
Communicating with Patients
You help patients understand hepatitis C testing by using clear and personal communication. Every patient has unique preferences, so you tailor your approach to fit their needs. Some patients prefer face-to-face conversations, while others respond better to written materials or phone calls. You use a multi-pronged strategy to reach everyone.
- Adjust your communication style for each patient.
- Use different methods, such as in-person talks, printed handouts, and phone calls.
- Recognize that no single method works for all patients.
You notice that some patients feel nervous or embarrassed about hepatitis C testing. Stigma can make them hesitate. You address these feelings by explaining that hepatitis C can affect anyone and that early testing helps protect their health. You answer questions and correct misconceptions about treatment. You encourage open discussion and reassure patients that their privacy matters.
Tip: You build trust by listening and responding to patient concerns. This helps patients feel comfortable with testing and follow-up care.
Integrating Testing into Practice
You make hepatitis C testing part of your daily routine by using efficient systems. Many clinics use electronic health record (EHR) templates to prompt staff to offer screening. Nurses often ask about hepatitis C during assessments and document consent before you see the patient. Some clinics use an opt-out policy, so nurses order tests unless patients say no. Patient navigators track positive results and help schedule follow-up appointments.
| Method Description | Details |
|---|---|
| Patient Navigator | Tracks HCV RNA positive results and schedules specialist appointments. |
| Customized EHR Template | Prompts staff to offer screening during routine visits. |
| Nursing Workflow | Nurses offer screening and document consent before physician interaction. |
| Opt-out Consent Policy | Nurses order tests unless patients object. |
You face barriers, such as billing issues, lack of onsite testing, and patient resistance. Some patients worry about costs or feel stigma. You overcome these challenges by educating staff about treatment costs and using reminders in the EHR. Clinics that added EMR alerts saw screening rates rise up to 15 times. Educational programs for staff also increased testing in community clinics.
Note: You improve screening rates by combining technology, education, and patient support. This helps more patients get tested and treated for hepatitis C.
You improve patient outcomes by following these steps for hepatitis C antibody testing:
- Start with antibody screening and confirm positives with HCV RNA testing.
- Use automated opt-out testing and educate your team to boost screening rates.
- Integrate routine screening into daily practice and use telehealth to keep patients engaged.
- Always provide timely follow-up and assess liver health before starting treatment.
Routine screening and proper follow-up help you prevent serious illness and support long-term health in your community.
FAQ
What does a hepatitis c virus antibody test show?
You use the antibody test to check if your patient has ever met the hepatitis c virus. This test finds antibodies in the blood. It does not show if the virus is active. You need more detection with pcr or other assays for current infection.
How soon after exposure can you detect the hepatitis c virus?
Detection depends on the window period. Antibodies may appear 8–11 weeks after meeting the hepatitis c virus. Early detection uses pcr or polymerase chain reaction. These assays find the virus before antibodies show up.
Why do you need both serology and pcr for hepatitis c virus detection?
Serology helps you find past exposure to the hepatitis c virus. You use pcr or polymerase chain reaction to see if the virus is active now. Combining both assays improves detection and increases the positive predictive value for current infection.
What is the sensitivity of serological assays for hepatitis c virus?
Sensitivity of serological assays for hepatitis c virus is high. Most tests find over 94% of cases. You use these assays for first detection. You confirm with pcr to make sure the virus is present.
Can a positive hepatitis c virus antibody test mean you do not have the virus now?
Yes. You may have met the hepatitis c virus before and cleared it. A positive result means past detection. You need pcr or other assays to check if the virus is still in your blood.

