News & Events
Which Is More Effective for Antibody-Mediated Rejection: Polyclonal or Monoclonal Antibodies

Current clinical guidelines and randomized controlled trials show that monoclonal antibodies often provide higher efficacy and safety in treating antibody-mediated rejection, especially in kidney and heart transplantation. Studies reveal that choosing the right treatment options can reduce allograft loss rates and improve long-term graft survival. The table below highlights important clinical measures for transplant patients:
| Metric | Value |
|---|---|
| Allograft loss rate | 37% |
| Response rates for pulse steroids/IVIG | eGFR: 27% |
| Response rates for steroids/IVIG/rituximab | eGFR: 66% |
Polyclonal vs monoclonal antibody therapies differ in their ability to control acute rejection and meet transplant recipient needs.
Key Takeaways
- Monoclonal antibodies often provide better efficacy and safety in treating antibody-mediated rejection, especially in kidney and heart transplants.
- Polyclonal antibodies act broadly to deplete lymphocytes quickly, making them useful for high-risk patients during induction therapy.
- Both antibody types can effectively manage acute rejection episodes, but monoclonal antibodies may lead to a higher risk of infections due to stronger immune suppression.
- Cost considerations are important; monoclonal antibodies like rituximab are generally less expensive than polyclonal options, making them more accessible.
- Doctors must evaluate patient-specific factors and follow guidelines to choose the best therapy for antibody-mediated rejection.
Antibody-Mediated Rejection

Definition
Antibody-mediated rejection (ABMR) occurs when the immune system attacks a transplanted organ. The body recognizes the new organ as foreign and produces antibodies against it. These antibodies target the donor organ’s cells and blood vessels. ABMR can happen soon after transplantation or many years later. Doctors often see ABMR in kidney and heart transplant recipients. ABMR is different from T cell-mediated rejection, which involves other immune cells. ABMR can lead to organ damage and loss if not treated quickly.
Pathophysiology
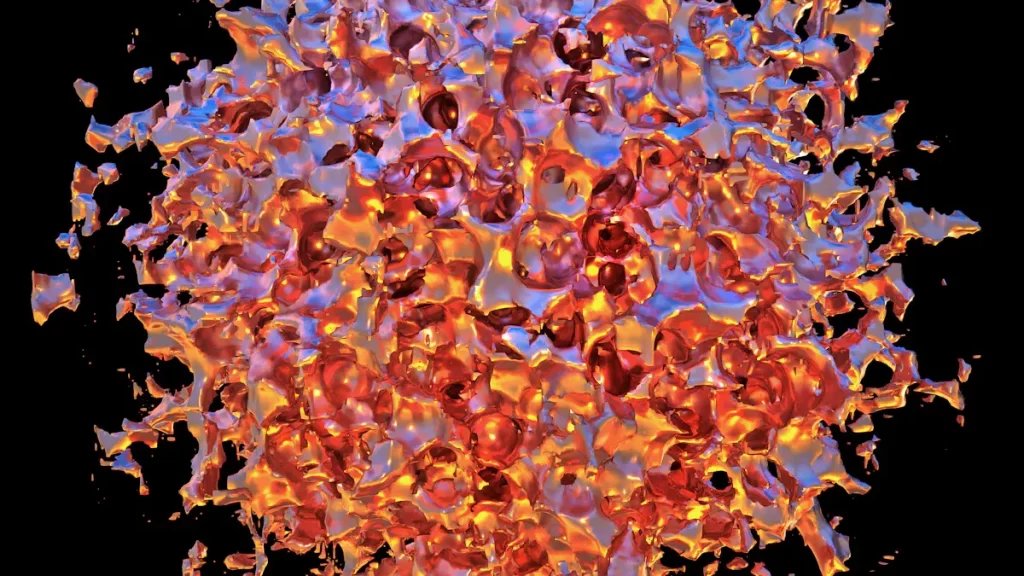
The process of antibody-mediated rejection involves several key steps. Donor-specific antibodies (DSA) play a central role. These antibodies attach to the cells of the transplanted organ. Natural killer (NK) cells also participate in the rejection process and contribute to graft injury. Doctors can see unique signs of ABMR under a microscope. For example, thrombotic microangiopathy and capillaritis are common in ABMR but not in T cell-mediated rejection. Gene expression signatures from graft biopsies help doctors understand how ABMR develops.
- Key mechanisms in ABMR:
- Donor-specific antibodies (DSA) attack the transplanted organ.
- Natural killer (NK) cells cause further injury.
- Thrombotic microangiopathy and capillaritis appear in tissue samples.
- Gene expression patterns reveal ABMR activity.
Treating ABMR in kidney and heart transplant patients presents many challenges. Doctors find it difficult to diagnose ABMR because biomarkers are complex. Distinguishing between preexisting and new donor-specific antibodies adds to the challenge. ABMR can occur years after transplantation, making long-term monitoring important. These factors make it hard to improve graft survival and develop effective treatment plans. Transplant teams must use careful strategies to manage ABMR and protect the transplanted organ.
Polyclonal vs Monoclonal Antibody: Mechanisms

Polyclonal Antibodies
Polyclonal vs monoclonal antibody therapies show important differences in how they work. Polyclonal antibodies come from the blood of animals that have been exposed to human lymphocytes. These antibodies target many types of immune cells. Doctors use polyclonal antibodies to deplete lymphocytes quickly. This action helps prevent the immune system from attacking the transplanted organ. In induction therapy, polyclonal antibodies like antithymocyte globulin (ATG) play a key role. ATG binds to T cells and removes them from the bloodstream. This process lowers the risk of acute rejection after transplantation.
Polyclonal vs monoclonal antibody therapies both aim to control the immune response, but polyclonal antibodies act broadly. They can cause side effects such as fever and chills because they affect many cell types. Induction therapy with polyclonal antibodies reduces the number of T cells and helps protect the new organ during the early period after surgery. Doctors often choose polyclonal antibodies for induction when patients have a high risk of rejection.
Monoclonal Antibodies
Monoclonal antibodies are designed to target specific immune cells or proteins. In polyclonal vs monoclonal antibody comparisons, monoclonal antibodies offer more precise control. These therapies block certain pathways that lead to antibody-mediated rejection. Induction therapy with monoclonal antibodies includes drugs like rituximab, which targets B cells, and eculizumab, which blocks complement activation. Induction with monoclonal antibodies can also involve IL2RA, which lowers the chance of acute rejection by about 30% compared to placebo.
| Mechanism of Action | Therapeutic Strategy |
|---|---|
| Inhibition of B cells | Mycophenolate mofetil, Rituximab |
| Inhibition of T cells | Mycophenolate mofetil, Steroids, Calcineurin inhibitors, ATG |
| Antibody removal | Plasmapheresis, Immunoadsorption, IVIG |
| Targeting plasma cells | Bortezomib |
| Complement inhibition | Eculizumab |
Induction therapy with monoclonal antibodies has become common in kidney transplantation. Doctors use induction to lower the risk of early acute rejection episodes. Induction therapy with ATG or IL2RA reduces the risk of rejection, but the benefit in standard-risk patients is smaller. Induction with monoclonal antibodies may only lower the absolute risk of acute rejection by 1-4%. Some studies show that eculizumab, a humanized monoclonal antibody, blocks C5 activation and reduces the incidence of antibody-mediated rejection in sensitized kidney transplant recipients. Induction therapy with monoclonal antibodies provides targeted action and may reduce side effects compared to polyclonal antibodies.
Induction therapy remains a key strategy in transplant medicine. Doctors must decide between polyclonal vs monoclonal antibody options based on patient risk and transplant type. Induction with monoclonal antibodies offers precise targeting, while polyclonal antibodies provide broad immune suppression. Both approaches play important roles in protecting transplanted organs.
Comparative Efficacy
Acute Rejection Episodes
Doctors often face challenges when managing acute rejection episodes in transplant patients. The treatment of acute rejection requires quick action to prevent organ damage. Comparative studies show that monoclonal antibodies, such as alemtuzumab, can reduce high-grade rejection events more effectively than polyclonal antibodies like rATG. Alemtuzumab provides better control of acute rejection episodes, but it may increase the risk of infections due to stronger immune suppression. The benefit of monoclonal antibodies in the treatment of acute rejection is clear in short-term outcomes, but long-term survival may be affected by complications.
| Study | Findings | Conclusion |
|---|---|---|
| Jaksch et al. | Alemtuzumab significantly reduced high-grade rejection events compared to rATG. | Alemtuzumab shows superior efficacy in acute rejection control. |
| Long-term outcomes | Increased risk of infections with prolonged immune suppression from monoclonal therapies. | Long-term survival benefits may be compromised despite better rejection control. |
Doctors use both polyclonal and monoclonal antibodies when steroids fail to reverse acute rejection episodes. These therapies show higher success rates than steroids alone. In cases of steroid-resistant acute cellular rejection, anti-T cell antibodies like ATG become the main option. Alemtuzumab also helps reverse steroid-resistant rejection, but more studies are needed to compare it with other agents. Polyclonal and monoclonal antibodies can rescue grafts that seem irreparably damaged, but they also cause side effects such as fever and infusion reactions.
Kidney Transplant Recipients
Kidney transplant recipients often experience acute rejection episodes, especially in the first year after surgery. The treatment of acute rejection in these patients relies on both polyclonal and monoclonal antibodies. Studies show that antibody therapies are more effective than steroids in reversing acute rejection and preventing treatment failure. The success rate for antibody therapy in reversing acute rejection episodes is higher than with steroids. Doctors see a benefit in using antibody therapies for kidney transplant recipients, but they must watch for side effects and infections.
| Therapy Type | Success Rate (RR) | 95% CI | Certainty Level |
|---|---|---|---|
| Antibody vs. Steroid (reversal) | 0.50 | 0.30 to 0.82 | Moderate |
| Antibody vs. Steroid (prevention) | 0.70 | 0.50 to 0.99 | Moderate |
| Antibody (graft loss prevention) | 0.80 | 0.57 to 1.12 | Low |
| Muromonab-CD3 vs. ATG/ALG | No benefit | N/A | N/A |
| Rituximab (reversal) | 0.94 | 0.54 to 1.64 | N/A |
| Rituximab (graft loss/death) | 1.0 | 0.23 to 4.35 | N/A |

Doctors see that both polyclonal and monoclonal antibodies help prevent treatment failure in kidney transplant recipients. The benefit of antibody therapy is most clear in patients who do not respond to steroids. However, treatment failure can still occur, especially if the patient develops severe side effects or infections. Doctors must balance the benefit of rejection control with the risk of complications.
Heart Transplantation
Heart transplantation presents unique challenges in the treatment of acute rejection. Acute rejection episodes can lead to treatment failure and loss of the transplanted heart. Doctors use both polyclonal and monoclonal antibodies to manage these episodes. Studies show that antibody therapies provide better outcomes than steroids alone. The benefit of antibody therapy in heart transplantation includes improved graft survival and lower rates of treatment failure.
Doctors often choose monoclonal antibodies for heart transplantation when patients have high risk of acute rejection episodes. These therapies target specific immune cells and help prevent treatment failure. However, the risk of infections and other side effects remains a concern. Polyclonal antibodies also play a role in the treatment of acute rejection, but they act more broadly and may cause more side effects.
Doctors must consider the benefit of antibody therapy against the risk of treatment failure and complications. Both polyclonal and monoclonal antibodies are more effective than steroids for acute cellular rejection in heart transplantation. The choice of therapy depends on patient risk, history of rejection, and potential for side effects.
Safety and Side Effects
Immediate Reactions
Doctors observe that both polyclonal and monoclonal antibody therapies can cause immediate reactions after administration. These reactions often occur within the first few hours. The most common symptoms include fever, chills, and malaise. Patients may also experience headaches, pain, and nausea. Some reactions are more severe, such as type I hypersensitivity, which can lead to urticaria, angioedema, or even anaphylaxis. Infusion-related reactions may present with flushing, hypotension, chest pain, or dyspnea. The table below summarizes these reactions:
| Type of Reaction | Description |
|---|---|
| Type I Hypersensitivity | IgE-mediated, immediate onset (1-2 hours), symptoms include urticaria, angioedema, anaphylaxis. |
| Infusion-related reactions | Fever, flushing, hypotension, dyspnea, chest pain; true hypersensitivity if angioedema or urticaria present. |
Patients receiving polyclonal antibodies often report fever, chills, malaise, and shaking chills. Severe systemic inflammatory responses can also occur. These symptoms require careful management to ensure patient safety.
- Common symptoms with polyclonal antibody therapy:
- Fever
- Chills
- Malaise
- Headache
- Pain
- Nausea
- Tachycardia
- Dyspnea
Infection Risk
Both polyclonal and monoclonal antibody therapies increase the risk of infection. These immunosuppressive agents lower the body’s ability to fight off viruses, fungi, and parasites. Doctors see a higher incidence of opportunistic infections in transplant recipients who receive these therapies. Monoclonal antibodies also carry specific risks for malignancies, such as post-transplant lymphoproliferative disorder (PTLD). The table below compares infection risks:
| Therapy Type | Infection Risk |
|---|---|
| Polyclonal Antibodies | Increased incidence of opportunistic infections, including viral, fungal, and parasitic infections. |
| Monoclonal Antibodies | Similar increased incidence of opportunistic infections, with specific risks for malignancies like PTLD. |
Effective management of infection risk is essential for maintaining a positive safety profile in transplant patients. Doctors monitor patients closely and adjust immunosuppressive regimens to reduce complications.
Tolerability
Clinical studies show that both polyclonal and monoclonal antibodies have a favorable safety profile. Most patients tolerate these immunosuppressive therapies well. Adverse events are usually mild to moderate. Doctors report no significant safety concerns in published studies. The table below outlines tolerability profiles:
| Type of Antibody | Tolerability Profile | Adverse Events | Severity Classification |
|---|---|---|---|
| Polyclonal | Well-tolerated | Mild to moderate | Mild, Moderate |
| Monoclonal | Well-tolerated | Mild to moderate | Mild, Moderate |
| Both | No significant safety concerns reported | Similar adverse effects between treatment and placebo groups | Mild to moderate adverse events observed |
Doctors consider the safety profile and tolerability when choosing immunosuppressive therapies for transplant management. They aim to balance effective rejection control with minimal side effects. Careful management of immunosuppressive regimens helps maintain patient safety and improve outcomes.
Practical Considerations
Cost
Transplant teams must consider the cost of polyclonal and monoclonal antibodies when planning treatment. The price of each therapy can affect hospital budgets and patient access. Polyclonal and monoclonal antibodies have different costs per dose. The table below shows the average cost for each therapy:
| Therapy Type | Average Cost (per dose) |
|---|---|
| Polyclonal (IVIG) | $10,500 – $20,000 |
| Monoclonal (Rituximab) | $3,384 |
Polyclonal and monoclonal antibodies both play a role in induction therapy. Basiliximab is often used because it offers a cost-effective option for many patients. Hospitals see that antibody-based induction therapy provides better outcomes and lower costs than no induction. Depletional induction, especially with rabbit anti-thymocyte globulin, gives the best balance between cost and effectiveness in kidney transplantation. Basiliximab helps reduce expenses while maintaining good results.
- Antibody-based induction therapy improves outcomes and lowers costs.
- Depletional induction with rabbit anti-thymocyte globulin is cost-effective for kidney transplants.
Availability
The availability of polyclonal and monoclonal antibodies depends on several factors. Hospitals must look at social determinants of health, support systems, and health disparities. The table below explains these factors:
| Factor | Description |
|---|---|
| Social Determinants of Health | Race, language, and ethnicity affect acceptance of monoclonal antibody therapies. |
| Social Support Systems | Patients with partners or religious groups accept therapies more often due to strong support. |
| Health Disparities | Underrepresented groups decline therapy more often because of mistrust or misinformation. |
Basiliximab is available in most hospitals and clinics. Doctors choose basiliximab for patients who need reliable access to therapy. Polyclonal and monoclonal antibodies may not be available in every healthcare setting. Hospitals in rural areas sometimes have limited supplies. Social support helps patients accept basiliximab and other therapies.
Administration
Doctors must follow strict protocols when giving polyclonal and monoclonal antibodies. Basiliximab requires careful dosing and monitoring. Nurses watch for side effects during and after administration. Hospitals use special equipment to deliver basiliximab safely. Polyclonal and monoclonal antibodies need close monitoring to prevent complications. Doctors check vital signs and watch for allergic reactions. Basiliximab is easy to administer and has a low risk of severe reactions. Nurses find basiliximab simple to use compared to other therapies.
Tip: Hospitals should train staff to recognize side effects and respond quickly. Proper administration of basiliximab and other antibody therapies improves patient safety.
Polyclonal and monoclonal antibodies require careful management. Basiliximab stands out for its ease of use and safety profile. Hospitals benefit from using basiliximab in induction therapy for kidney and heart transplantation.
Clinical Decision-Making
Patient Factors
Doctors must look at many patient factors before choosing a therapy for antibody-mediated rejection. Age, medical history, and type of transplant all play important roles. Some patients have a higher risk of rejection because of previous transplants or strong immune responses. Others may have health problems that make certain treatments unsafe. The risk-benefit ratio helps doctors decide which therapy is best for each patient. They weigh the chance of stopping rejection against possible side effects. For example, a patient with a high risk of infection may need a different approach than one with a strong immune system.
Doctors also consider how well a patient can follow treatment plans. Support from family or friends can improve outcomes. Surveillance protocols, such as donor-derived cell-free DNA and gene profile testing, help doctors detect rejection early. These tools allow for quick changes in therapy, improving the risk-benefit ratio for each patient. Induction immunosuppression may be chosen for patients with high risk of rejection, but doctors must watch for side effects.
Tip: Doctors should talk with patients about their preferences and concerns. This helps build trust and improves treatment success.
Guidelines
Expert guidelines help doctors choose the right therapy for antibody-mediated rejection. Most guidelines recommend using the risk-benefit ratio to guide decisions. Doctors follow protocols from transplant societies and review new research often. Induction immunosuppression is suggested for patients with high risk of rejection, but not for everyone. Ongoing clinical trials offer new options for therapy, especially for kidney transplant recipients.
| Guideline Principle | Recommendation |
|---|---|
| Risk-benefit ratio | Use to guide therapy selection |
| Induction immunosuppression | Recommended for high-risk patients |
| Surveillance protocols | Use for early detection and therapy adjustment |
| Emerging data | Review new studies and update practices |
Doctors must keep learning as new data becomes available. Advances in understanding antibody-mediated rejection have led to better therapies. Long-term survival rates remain low, so doctors need to adjust treatments as new evidence appears. Chronic active antibody-mediated rejection is still hard to treat, and no therapy has shown strong results in large trials. Doctors should review ongoing studies and update their practices to improve patient outcomes.
Current evidence and clinical guidelines show monoclonal antibodies often provide better control of antibody-mediated rejection in transplantation. The table below highlights key differences:
| Aspect | Monoclonal Antibodies (mAbs) | Polyclonal Antibodies (pAbs) |
|---|---|---|
| Efficacy | Significant clinical acclaim with over 20 mAbs in use; notable benefits in COVID-19 treatment | N/A |
| Safety | Associated with adverse events but overall favorable safety profile; 0.2% adverse events in COVID-19 mAb treatments | N/A |
| Manufacturing Challenges | High production costs due to complex manufacturing processes; potential for 20%-40% cost savings with continuous manufacturing | N/A |
Clinicians should use CYP3A5 testing, therapeutic drug monitoring, and multigene panel testing to guide therapy for kidney and heart transplantation. Monitoring for adverse reactions, including hepatotoxicity and immune responses, remains essential. Regular updates to practice based on new research help improve transplantation outcomes.
FAQ
What are antilymphocyte antibodies and how do they work in transplantation?
Antilymphocyte antibodies target and remove specific immune cells called lymphocytes. Doctors use these antibodies to prevent the body from attacking a transplanted organ. This therapy helps lower the risk of rejection and improves transplant success rates.
Are antilymphocyte antibodies used for both kidney and heart transplants?
Doctors use antilymphocyte antibodies in both kidney and heart transplantation. These antibodies help control the immune response and reduce the chance of acute rejection. Their use depends on patient risk and transplant type.
What side effects can occur with antilymphocyte antibodies?
Patients may experience fever, chills, or malaise after receiving antilymphocyte antibodies. Some may develop allergic reactions or infections. Doctors monitor patients closely to manage these side effects and ensure safety during treatment.
How do antilymphocyte antibodies compare to monoclonal antibodies in cost?
Antilymphocyte antibodies often cost more per dose than some monoclonal antibodies. Hospitals consider cost when choosing therapy. Basiliximab, a monoclonal antibody, offers a cost-effective option for many transplant patients.
Can children receive antilymphocyte antibodies after transplantation?
Doctors prescribe antilymphocyte antibodies for children who need organ transplants. These therapies help prevent rejection in pediatric patients. Doctors adjust doses based on age and weight to ensure safety and effectiveness.