News & Events
3 Key Ways Ro Antibody Impacts You in 2025
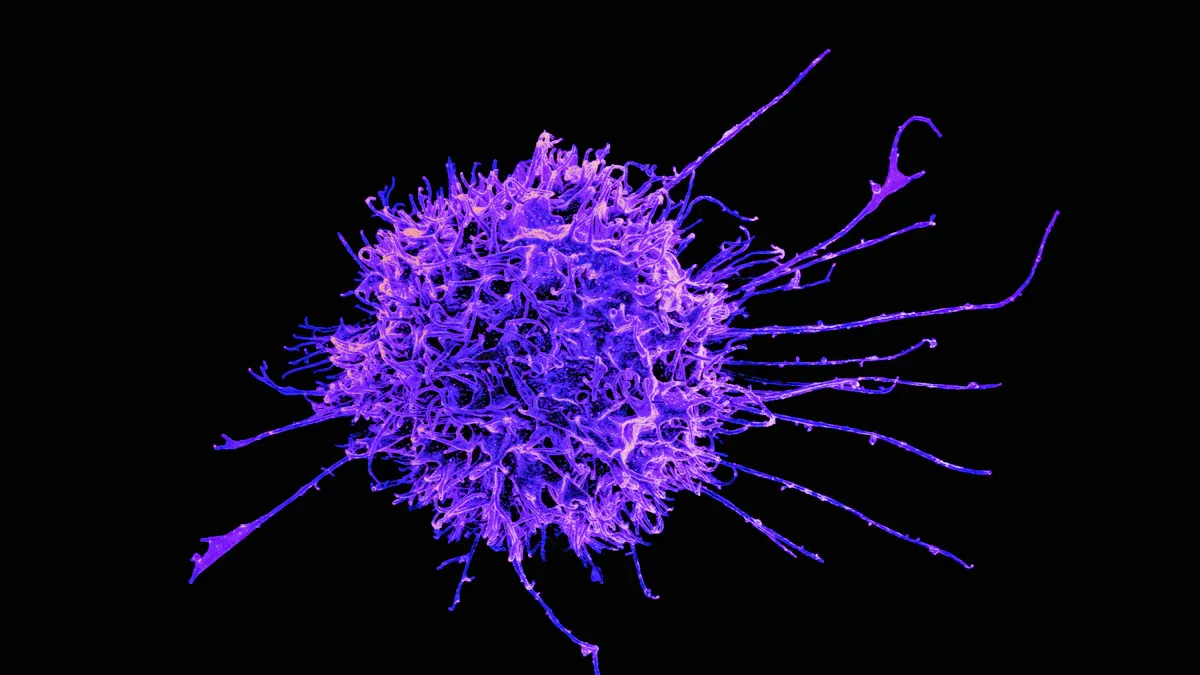
Ro antibody testing changes the lives of many patients in 2025. Doctors see new patterns in clinical outcomes, especially for those with autoimmune conditions. The data below shows how different health issues appear in people with positive tests.
| Outcome Type | Pooled Estimate Rate |
|---|---|
| Termination of Pregnancy | 4% |
| Spontaneous Abortion | 5% |
| Preterm Labor | 26% |
| Cesarean Operation | 50% |
| Perinatal Death | 4% |
| Intrauterine Growth Retardation | 3% |
| Endocardial Fibroelastosis | 6% |
| Dilated Cardiomyopathy | 6% |
| Congenital Heart Block | 7% |
| Congenital Heart Block Recurrence | 12% |
| Cutaneous Neonatal Lupus Erythematosus | 19% |
| Hepatobiliary Disease | 12% |
| Hematological Manifestations | 16% |
Understanding these risks helps both doctors and families make better choices for care.
Key Takeaways
- Ro antibody testing enables early detection of autoimmune diseases, allowing for timely monitoring and treatment, which can improve patient outcomes.
- Understanding the risks associated with anti-Ro antibodies helps doctors and families make informed decisions about care, especially during pregnancy.
- Regular follow-up and communication between patients and healthcare providers are essential for managing autoimmune diseases effectively and adapting treatment plans as needed.
- Lifestyle changes, such as avoiding competitive sports and adjusting medications, can significantly reduce complications for patients with anti-Ro antibodies.
Ro Antibody in Diagnosis
Early Detection
Doctors use anti-ro antibodies to help identify autoimmune diseases early. These antibodies play a key role in diagnosing connective tissue diseases such as SLE and primary Sjögren’s syndrome. Many patients show anti-ro antibodies before they develop clear symptoms. This early presence allows doctors to start monitoring and treatment sooner, which can improve outcomes for patients.
Early detection of anti-ro antibodies helps doctors recognize autoimmune diseases before major symptoms appear. This step can prevent severe complications in patients with SLE or primary Sjögren’s syndrome.
Researchers have found several important facts about anti-ro antibodies and early detection:
- The presence of anti-ro/SSA antibodies is a critical criterion in the 2016 ACR-EULAR classification for Sjögren’s syndrome.
- Anti-Ro60/SSA positivity is frequently associated with SLE, with a study showing it as the most common diagnosis in patients with this antibody.
- The positive predictive value of anti-Ro60/SSA antibodies is notably high in primary Sjögren’s syndrome, indicating their importance in early detection.
Doctors rely on these antibodies to guide the diagnosis of connective tissue diseases. Many patients with SLE or primary Sjögren’s syndrome test positive for anti-ro antibodies. This helps doctors confirm the diagnosis and begin treatment plans tailored to each patient.
ANA Patterns
Doctors often use antinuclear antibodies (ANA) tests to screen for autoimmune diseases. The patterns seen in ANA tests can give clues about the type of disease present. Anti-ro antibodies often create specific ANA patterns, which help doctors identify connective tissue diseases like SLE and primary Sjögren’s syndrome.
The detection and interpretation of ANA patterns can differ by region. Some labs use advanced technology to spot subtle differences in ANA patterns. This helps doctors make a more accurate diagnosis for patients with suspected autoimmune diseases.
The diagnostic accuracy of anti-ro antibodies varies by assay type. The table below shows the sensitivity and specificity of different tests for connective tissue diseases:
| Assay Type | Sensitivity | Specificity |
|---|---|---|
| Phadia SSA | 69% | 100% |
| Anti-Ro 52 | N/A | N/A |
| Anti-Ro 60 | N/A | N/A |
| Anti-La | N/A | N/A |
Doctors use these results to choose the best test for each patient. High specificity means that a positive result almost always points to a true case of SLE or primary Sjögren’s syndrome. This helps avoid misdiagnosis and ensures patients receive the right care.
The significance of ANA patterns and anti-ro antibodies in diagnosing autoimmune disorders cannot be overstated. These tools help doctors find disease early, confirm the diagnosis, and guide treatment for patients with connective tissue diseases. Understanding these patterns improves the clinical approach to autoimmune diseases and supports better outcomes for patients.
Clinical Implications of Anti-Ro Antibodies

Risk in Patients with SLE and Sjögren’s
The clinical significance of anti-ro antibodies stands out in patients with systemic lupus erythematosus and primary Sjögren’s syndrome. These antibodies help doctors understand the diagnostic and prognostic value for different connective tissue diseases. Many patients with anti-ro antibodies show unique patterns of disease.
- In primary Sjögren’s syndrome, 50% to 90% of patients test positive for anti-ro antibodies.
- In systemic lupus erythematosus, 30% to 40% of patients have these antibodies.
Doctors see that patients with anti-ro antibodies often have different symptoms than those without these antibodies. The table below shows how the presence of anti-ro antibodies changes the risk for certain features in SLE:
| Finding | Anti-Ro+ SLE | Anti-Ro− SLE |
|---|---|---|
| Sicca Syndrome | More common | Less common |
| Overlap with other rheumatological entities | More common | Less common |
| Arthritis | Less common | More common |
| Need for bolus corticosteroids | Less common | More common |
| Current SLICC | Less common | More common |
Doctors notice that cutaneous and musculoskeletal symptoms appear more often in patients with anti-ro antibodies. These patients may also have milder forms of childhood-onset SLE. Secondary Sjögren’s syndrome rarely appears, even when antibody levels are similar.
The clinical significance of anti-ro antibodies helps doctors predict which organs might be affected. This information guides treatment and monitoring for patients with connective tissue diseases.
Interstitial Lung Disease and Pulmonary Hypertension
Anti-ro antibodies, especially anti-Ro52, play a major role in the development of interstitial lung disease in autoimmune diseases. Research shows that patients with anti-ro antibodies face a much higher risk of lung problems. In idiopathic inflammatory myopathies, the presence of anti-Ro52 antibodies increases the risk of interstitial lung disease eight-fold. When these antibodies combine with other myositis-specific antibodies, the risk rises to twenty-fold.
A systematic review found that anti-Ro52 positivity links to interstitial lung disease across several autoimmune diseases. The odds ratios show a strong association:
- Idiopathic inflammatory myopathies: OR = 3.08
- Systemic lupus: OR = 2.43
- Sjögren’s syndrome: OR = 1.77
- Systemic sclerosis: OR = 1.71
- Mixed connective tissue disease: OR = 3.34
Patients with anti-ro antibodies also face a higher chance of rapidly progressive interstitial lung disease, especially in myopathy. The odds ratio for this severe form is 2.69. These findings highlight the clinical significance of anti-ro antibodies in predicting lung involvement.
Doctors have also reported cases where patients with anti-ro antibodies and Sjögren’s syndrome develop pulmonary hypertension. This possible link shows the need for careful monitoring of lung and heart health in patients with anti-ro antibodies.
Pregnancy and Congenital Heart Block
The clinical significance of anti-ro antibodies becomes very important during pregnancy. Women with these antibodies need special care because of the risk of congenital heart block in their babies. The diagnostic and prognostic value of anti-ro antibodies helps doctors identify which pregnancies need closer monitoring.
- Women with active disease and high antibody titers may have a slightly higher risk of congenital heart block.
- Isolated SSB-positive titers do not significantly increase the risk for congenital heart block.
- The risk of fetal complete atrioventricular block in first-time pregnancies with anti-ro antibodies is about 2%.
- If a previous pregnancy had fetal heart block, the risk rises to 18% to 20% in future pregnancies.
Doctors recommend that women with known positive anti-ro antibodies see a specialized fetal medicine unit. A multidisciplinary team should provide counseling about risks and treatment options. Intensive monitoring is needed between 16 and 26 weeks of pregnancy, with weekly fetal echocardiography. Asymptomatic mothers with positive anti-ro or anti-La antibodies should also have frequent echocardiograms, especially from 18 to 24 weeks. The American Heart Association suggests serial exams from 16 to 28 weeks.
Regular screening and early detection of anti-ro antibodies in pregnant women can help prevent serious complications for both mother and baby.
The clinical significance of anti-ro antibodies in pregnancy highlights the need for careful planning and monitoring. Doctors use this information to protect the health of both patients and their children.
Management Strategies for Patients
Monitoring and Follow-Up
Effective monitoring helps patients with anti-ro antibodies manage autoimmune diseases and connective tissue diseases. Doctors recommend several strategies to track disease activity and prevent complications:
- Home monitoring allows pregnant women with anti-ro antibodies to check fetal heart rates several times each day.
- Many experts suggest weekly fetal echocardiography, while others recommend bi-weekly checks.
- No single monitoring plan fits all patients, so doctors adjust follow-up based on individual needs.
| Evidence Summary | Importance of Follow-Up |
|---|---|
| New autoimmune diseases and skin disease progress are common in Ro/SSA-positive patients in the short term. | Regular follow-up is crucial for monitoring the dynamic nature of the disease and potential new conditions. |
| Development of new diagnoses such as CLE, RA, SS, SLE, vasculitis, and psoriasis arthritis within 2 years. | Highlights the need for ongoing clinical follow-up and collaboration between specialists for effective management. |
Doctors stress the importance of regular follow-up for patients with anti-ro antibodies. New autoimmune diseases can develop quickly, so ongoing clinical care supports early detection and treatment.
Lifestyle and Medication
Lifestyle changes and medication adjustments play a key role in the management of anti-ro antibody-positive patients. Doctors encourage patients to make choices that lower the risk of complications from connective tissue diseases.
| Recommendation | Description |
|---|---|
| Avoid competitive sports | Reduces the risk of arrhythmia triggers. |
| Discontinue medications that prolong QT interval | Helps in managing arrhythmia risk effectively. |
| Use beta-adrenergic blockers | Suggested to lower the risk of arrhythmias. |
Doctors also follow guidelines from major rheumatology organizations:
| Guideline Source | Recommendation |
|---|---|
| EULAR/ACR | Testing for anti-SSA (anti-ro) antibodies is emphasized in specific patient populations, particularly those planning pregnancy or with suspected autoimmune diseases. |
| 2020-ACR-Guideline | Screen for anti-SSA and anti-SSB in all patients with rheumatoid arthritis who are planning pregnancy or are pregnant. |
Medication plans may change as new symptoms appear. Doctors work closely with patients to adjust treatments for SLE, SS, and other connective tissue diseases.
Communication with Clinicians
Clear communication between patients and clinicians supports better outcomes in clinical practice. Doctors face challenges because anti-ro antibodies can cause different symptoms in each patient. Individualized care plans help address these differences.
- Individualized treatment is important for pregnancies complicated by autoimmune diseases.
- Counseling before and during pregnancy can improve outcomes.
- Specialized health professionals, including obstetricians, should manage care throughout pregnancy and after childbirth.
- Risk stratification considers disease activity, medication, and modifiable risks.
- Patients and doctors develop tailored treatment plans together.
- Multidisciplinary teams provide close monitoring and management during pregnancy.
- Continuous adjustments to care plans are needed as pregnancy progresses.
Good communication and teamwork help patients with anti-ro antibodies manage their disease and improve quality of life.
Doctors use clinical decision-making to guide management and adjust care as needed. The significance of anti-ro antibodies in connective tissue diseases means that every patient needs a plan that fits their unique situation.
Ro antibody testing shapes patient care in 2025 by enabling early detection, guiding clinical decisions, and supporting proactive management. Recent studies show that anti-ro52 antibody links to more severe outcomes in stroke patients, highlighting the significance of antibody profiles. The table below shows how different antibody types affect patient outcomes and management:
| Antibody Profile | Clinical Implications | Patient Outcomes |
|---|---|---|
| Anti-Ro60 and Anti-Ro52 | Higher likelihood of dryness of mouth and eyes in SS patients | Improved diagnosis and targeted management |
| Solo Anti-Ro52 | Increased suspicion for IM and malignancies | Enhanced monitoring for ILD and PAH |
| Isolated Anti-Ro52 | Higher possibility of ILD and PAH | Better risk stratification |
Ongoing conversations between patients and healthcare teams help everyone stay informed about advances in anti-ro antibody research and care.
FAQ
What does a positive anti-Ro antibody test mean?
A positive anti-Ro antibody test shows that the body makes antibodies linked to autoimmune diseases. Doctors use this result to help diagnose conditions like lupus or Sjögren’s syndrome.
Can anti-Ro antibodies affect pregnancy?
Yes. Women with anti-Ro antibodies have a higher risk of complications, such as congenital heart block in babies. Doctors recommend regular monitoring and specialized care during pregnancy.
How often should patients with anti-Ro antibodies see their doctor?
Patients should visit their doctor regularly. Most experts suggest check-ups every few months. Doctors may increase visits if symptoms change or new risks appear.
Are anti-Ro antibodies linked to lung problems?
Anti-Ro antibodies, especially anti-Ro52, raise the risk of interstitial lung disease. Doctors watch for breathing issues and may order lung tests to catch problems early.
What lifestyle changes help patients with anti-Ro antibodies?
Doctors advise patients to avoid competitive sports and stop medicines that prolong the QT interval. Beta-blockers may help lower arrhythmia risk. Healthy habits support better outcomes. 🏃♂️🍎