News & Events
Exploring the Link Between Specific Antibody Deficiency and Graft Outcomes
Specific antibody deficiency increases the risk of poor outcomes for transplant patients. Doctors see higher rates of antibody-mediated rejection in those with this condition. Many transplant recipients show signs of hypogammaglobulinemia, with 45% affected overall and 40% in kidney transplant patients. Children experience lower rates compared to adults.
- Patients who develop donor-specific antibodies after transplant have a lower 10-year graft survival rate, dropping from 96% to 57%.
- Doctors often detect these antibodies before the organ shows problems.
Transplant professionals must watch for specific antibody deficiency and adjust treatments. Careful monitoring and personalized therapy help protect graft function.
Key Takeaways
- Specific antibody deficiency increases the risk of poor transplant outcomes. Regular monitoring for this condition is essential for better patient care.
- Patients with donor-specific antibodies face significantly lower graft survival rates. Early detection and intervention can improve long-term outcomes.
- Immunoglobulin therapy can help manage antibody-mediated rejection. This treatment supports the immune system and improves graft survival.
- Transplant teams should focus on personalized treatment plans. Tailored strategies enhance monitoring and management of antibody responses.
- Ongoing research aims to improve graft survival rates. New therapies and better monitoring techniques are crucial for future advancements in transplantation.
Specific Antibody Deficiency Overview
Definition and Types
Specific antibody deficiency plays a critical role in transplantation. Doctors define this condition as the presence of normal immunoglobulin levels but a poor antibody response to certain vaccines, especially those containing polysaccharide antigens. In transplantation, this means that even when a patient has normal antibody levels, the immune system cannot produce effective antibodies against specific bacteria. This problem often leads to repeated respiratory infections after transplant.
Note: There is no universal agreement on how to diagnose or treat specific antibody deficiency in transplantation. This lack of consensus can make management challenging for transplant teams.
Transplant specialists recognize several types of antibody deficiencies. The most common type seen in transplantation is acquired hypogammaglobulinemia. This condition involves low immunoglobulin levels and increases the risk of infection after transplant. The table below summarizes the main type identified in transplant medicine:
| Type of Antibody Deficiency | Description | Associated Pathogens |
|---|---|---|
| Acquired Hypogammaglobulinemia (HGG) | Low immunoglobulin levels, leading to higher infection risk after transplant | Measles, Tetanus |
Transplantation teams must understand these types to provide the best care for patients.
Prevalence in Transplant Patients
Specific antibody deficiency appears frequently in transplantation. Studies show that many transplant recipients develop this problem after surgery. In kidney transplantation, about 40% of patients experience some form of antibody deficiency. The overall rate in transplantation reaches nearly 45%. Children who undergo transplantation have lower rates than adults, but the risk remains significant.
Transplant professionals see that patients with specific antibody deficiency face more infections and complications. These problems can threaten graft survival. Regular monitoring for antibody responses helps doctors detect issues early. Early detection allows for better management and improved outcomes in transplantation.
Clinical Impact of Specific Antibody Deficiency
Graft Outcomes
Specific antibody deficiency affects allograft outcomes in many ways. Transplantation teams see that patients with this deficiency often develop donor-specific antibodies. These antibodies target the transplanted organ and increase the risk of antibody-mediated rejection. Doctors find that both acute antibody-mediated rejection and chronic antibody-mediated rejection can occur. These conditions threaten the long-term function of the allograft.
Many studies show that donor-specific antibodies are common in transplantation. The presence of these antibodies links to poor allograft outcomes. Patients with donor-specific antibodies before transplantation, even with a negative crossmatch, face a higher risk of antibody-mediated rejection. Early monitoring of donor-specific antibodies after transplant helps doctors predict long-term allograft outcomes. Patients who clear donor-specific antibodies or show lower levels after transplantation have similar allograft outcomes to those who never develop these antibodies.
| Finding | Description |
|---|---|
| DSA Prevalence | Numerous studies link donor-specific antibody presence to poor graft outcomes. |
| Graft Survival | Renal recipients with donor-specific antibodies have lower graft survival rates at 3 and 5 years post-transplant. |
| AMR Impact | Episodes of antibody-mediated rejection lead to significantly lower renal allograft survival. |
| Long-term Survival | Effective reduction of donor-specific antibody levels correlates with superior long-term survival. |
Doctors also see that antibody-mediated vascular rejection can damage the blood vessels of the transplanted organ. This damage increases the risk of allograft loss. Chronic lung allograft dysfunction is another problem linked to specific antibody deficiency. Patients with chronic lung allograft dysfunction often have ongoing donor-specific antibody production. This ongoing immune response leads to chronic antibody-mediated rejection and a higher risk of allograft loss.
Transplantation teams use regular monitoring to detect donor-specific antibodies early. They know that early detection and treatment of antibody-mediated rejection improve clinical outcomes. Patients with specific antibody deficiency need close follow-up to prevent antibody-mediated vascular rejection and chronic lung allograft dysfunction. These steps help reduce the risk of allograft loss and improve long-term survival.
Note: Patients who receive immunoglobulin therapy after transplantation may have a lower rate of re-infection and faster recovery of normal antibody levels. This therapy can support better allograft outcomes.
Infection and Rejection Risk
Specific antibody deficiency increases the risk of infection and the risk of rejection after transplantation. Patients with low antibody levels or poor antibody responses face more infections. These infections include viral, bacterial, and fungal diseases. Doctors see that hypogammaglobulinemia, a type of antibody deficiency, raises the risk of infection in transplant patients.
| Evidence Type | Description |
|---|---|
| Hazard Ratio | HGG was significantly associated with infection (HR: 1.895, 95% CI: 1.871–1.920; p< 0.001) |
| Infection Type | Graft-related viral infection (HR: 1.152, 95% CI: 1.144–1.160; p< 0.001) |
Transplantation teams observe that immunodeficiency increases the risk of severe infections, such as HPV, in transplant patients. Both primary and acquired immunodeficiencies lead to worse clinical outcomes. Many solid organ transplant recipients develop hypogammaglobulinemia after transplantation. Low immunoglobulin levels link to poor post-transplant outcomes and a higher risk of allograft loss.
Doctors also note that antibody-mediated rejection is more likely when patients have specific antibody deficiency. Donor-specific antibodies can trigger acute antibody-mediated rejection and chronic antibody-mediated rejection. These immune responses cause antibody-mediated vascular rejection and chronic lung allograft dysfunction. The risk of allograft loss rises with each episode of antibody-mediated rejection.
Transplantation teams use immunoglobulin therapy to lower the risk of infection and the risk of rejection. Patients who receive this therapy after transplantation have a lower rate of re-infection and recover normal antibody levels faster. This approach helps protect against chronic lung allograft dysfunction and reduces the risk of allograft loss.
- Chronic lung allograft dysfunction remains a leading cause of late graft failure.
- Donor-specific antibody monitoring helps identify patients at risk for antibody-mediated vascular rejection.
- Early intervention can prevent chronic antibody-mediated rejection and improve allograft outcomes.
Doctors recommend regular monitoring for donor-specific antibodies and antibody-mediated rejection in all transplant patients. This strategy helps reduce the risk of allograft loss and supports better long-term clinical outcomes.
Antibody-Mediated Rejection Mechanisms
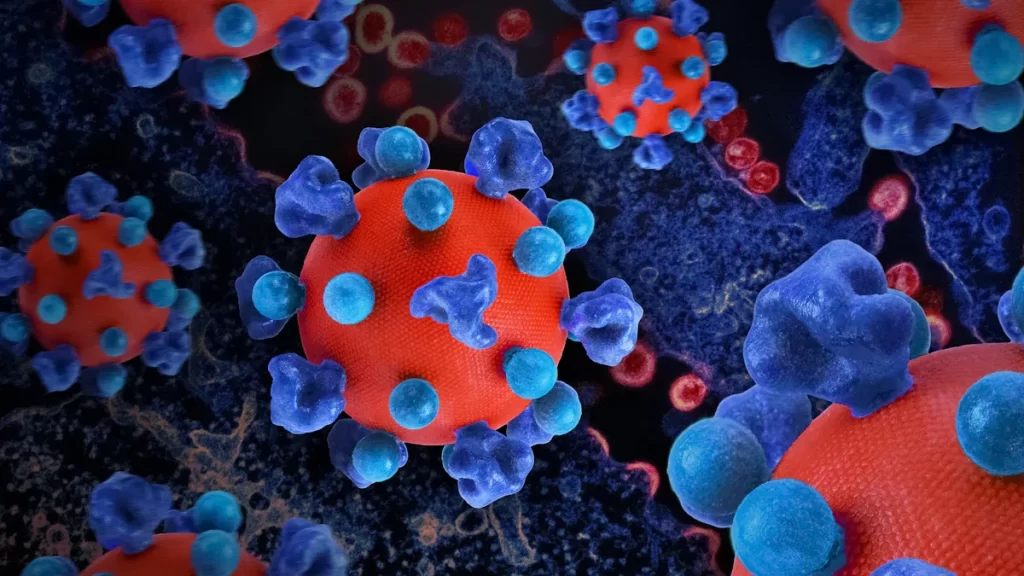
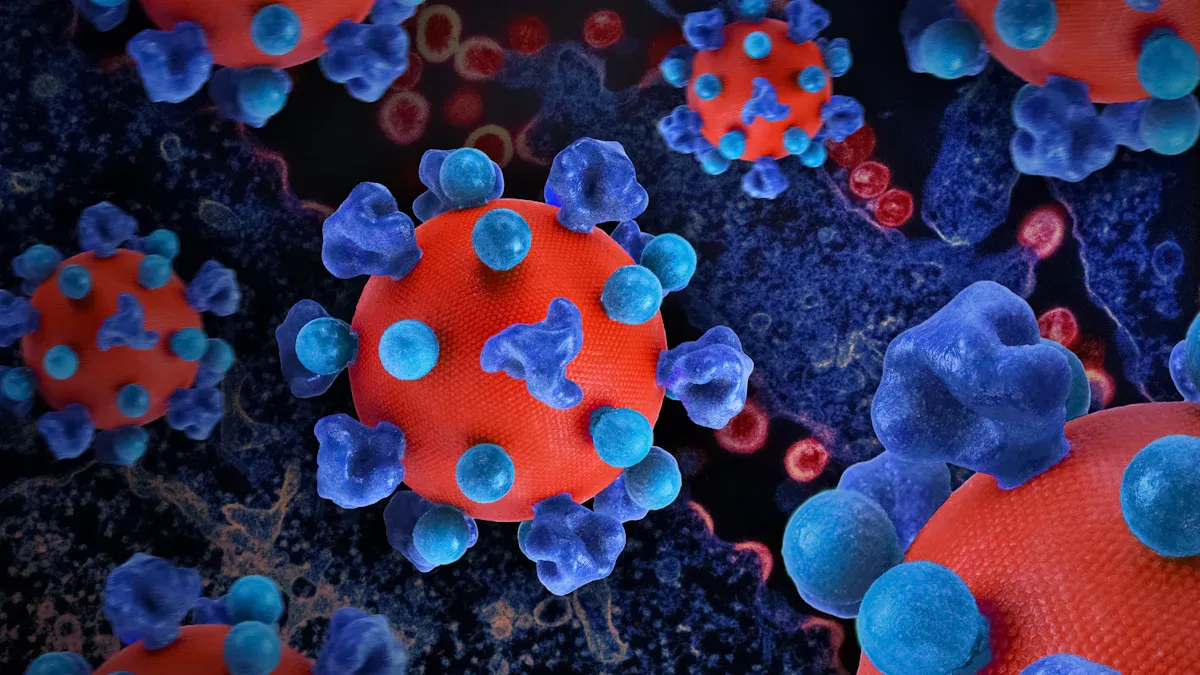
Donor-Specific Antibodies
Donor-specific antibodies play a central role in antibody-mediated rejection after transplantation. These antibodies develop when the immune system recognizes proteins from the transplanted organ as foreign. The body produces donor-specific antibodies that target these proteins. Doctors monitor patients for donor-specific antibodies because their presence signals a higher risk of antibody-mediated rejection.
Transplant teams use blood tests to detect donor-specific antibodies. These tests help identify patients who may develop antibody-mediated rejection. Donor-specific antibodies can appear before or after transplantation. When donor-specific antibodies bind to the organ, they start a chain reaction that leads to antibody-mediated injury. This process damages the transplanted tissue and can cause graft failure.
| Donor-Specific Antibody Feature | Impact on Transplant |
|---|---|
| Early detection | Allows prompt intervention |
| High levels | Increase risk of antibody-mediated rejection |
| Persistent presence | Signals ongoing immune attack |
Doctors focus on reducing donor-specific antibody levels to protect the graft. They use immunosuppressive drugs and other therapies to lower the risk of antibody-mediated rejection. Regular monitoring helps catch donor-specific antibodies early, improving long-term outcomes for transplant patients.
Complement Activation
Complement activation is a key process in antibody-mediated rejection. When donor-specific antibodies bind to the cells of the transplanted organ, they expose sites for complement proteins like C1q. This triggers a series of reactions known as the classical pathway. C1q activates enzymes called C1r and C1s, which split another protein, C4, into C4a and C4b. C4b attaches to the organ’s cells and forms C4d, a marker that doctors use to identify antibody-mediated rejection.
- Alloantibodies attached to endothelial cells start complement activation through C1q and MBL pathways.
- This activation causes injury to endothelial cells and leads to antibody-mediated graft rejection.
- Macrophages respond to complement activation by releasing inflammatory cytokines such as IL-1-α, IL-1-β, IL-6, and TNF-α.
Doctors look for C4d in tissue samples to confirm antibody-mediated rejection. The presence of C4d shows that complement activation has occurred. This process increases inflammation and damages the transplanted organ. Transplant teams use therapies to block complement activation and reduce the risk of antibody-mediated injury. Early detection and treatment help protect the graft and improve survival rates.
Heart Transplantation and SAD
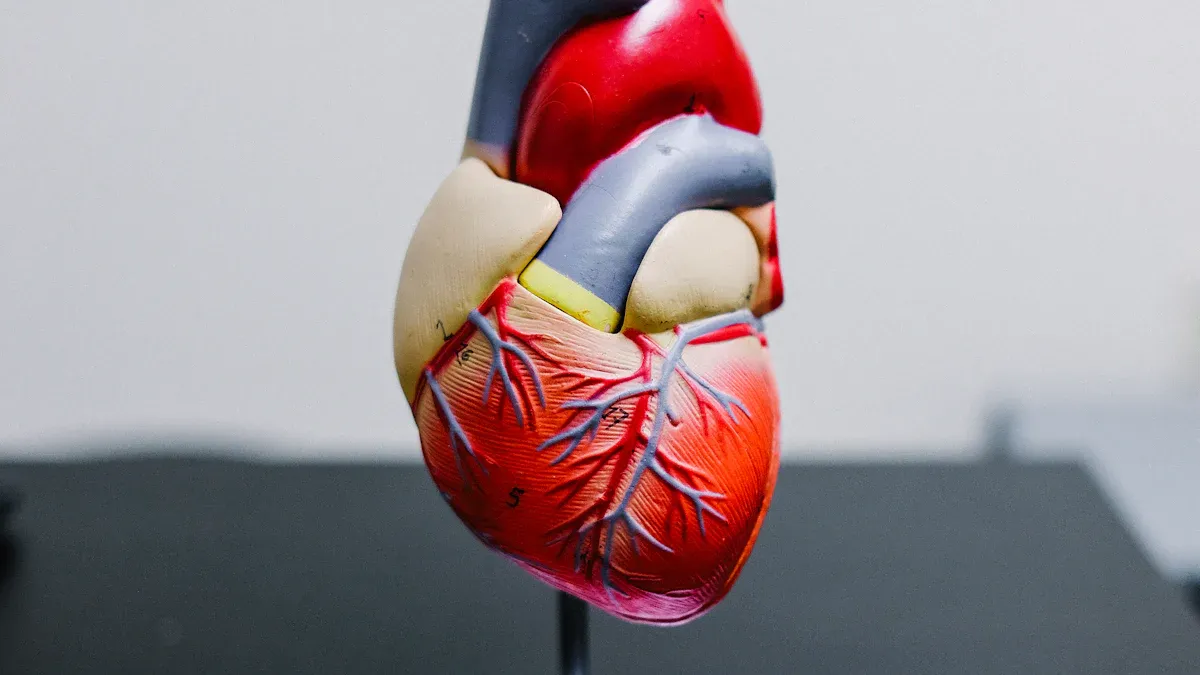
AMR in Heart Transplants
Heart transplantation offers hope to patients with severe heart disease. Doctors know that antibody-mediated rejection (AMR) remains a major challenge after transplant. Patients with specific antibody deficiency face a higher risk of AMR. The immune system may not respond well to infections, but it can still produce harmful antibodies against the new heart. These antibodies attack the transplanted organ and increase the risk of rejection.
Transplant teams see that AMR can happen early or late after heart transplantation. Some patients develop donor-specific antibodies that target the heart. These antibodies can cause swelling, damage blood vessels, and reduce heart function. Doctors monitor for signs of AMR because early detection helps prevent graft loss. The risk of AMR rises when patients have a history of infections or poor antibody responses.
Doctors use several strategies to lower the risk of AMR. They adjust immunosuppressive medications and may give immunoglobulin therapy. These treatments help control antibody levels and protect the transplanted heart. Transplantation teams work together to watch for changes in heart function and antibody levels. They know that quick action can save the graft and improve survival.
AMR remains a leading cause of late graft failure in heart transplantation. Early intervention and regular monitoring help reduce the risk of rejection.
Monitoring Strategies
Monitoring plays a key role in heart transplantation. Doctors use different tests to find antibody-mediated rejection early. They check for donor-specific antibodies and watch for changes in heart function. Regular testing helps doctors spot problems before they become serious.
Transplant teams recommend donor-specific antibody testing at 10 to 14 days after heart transplantation. This test identifies patients at high risk for AMR. Doctors also use molecular biomarkers, such as donor-derived cell-free DNA (dd-cfDNA), to detect rejection. These new tests may reduce the need for endomyocardial biopsy, which is invasive.
| Monitoring Strategy | Description |
|---|---|
| Donor-Specific Antibody Testing (DSA) | Identifies high-risk pAMR+/DSA+ patients; recommended at 10-14 days post-heart transplantation. |
| Molecular Biomarkers | Emerging tests like dd-cfDNA may allow rejection diagnosis without the need for biopsy. |
| Molecular Testing | Includes DSAs and/or dd-cfDNA for rejection diagnosis, potentially reducing the need for biopsy. |
Doctors use these strategies to lower the risk of graft loss. They know that regular monitoring and early treatment improve outcomes in heart transplantation. Transplantation teams teach patients about the importance of follow-up visits and testing. They encourage patients to report any symptoms quickly. This approach helps protect the transplanted heart and reduces the risk of rejection.
Diagnosis and Monitoring
Detecting Donor-Specific Antibodies
Doctors use several methods to detect donor-specific antibodies in transplant patients. These antibodies serve as important biomarkers for predicting antibody-mediated rejection and graft loss. The presence of donor-specific antibodies before transplantation can lead to immediate rejection. Patients who develop new donor-specific antibodies after surgery face a higher risk of late rejection and chronic antibody-mediated injury. The characteristics of donor-specific antibodies, such as HLA classes and IgG subclasses, help doctors determine the risk for each patient.
Donor-specific antibodies (DSAs) are critical biomarkers for predicting antibody-mediated rejection and graft loss in transplant patients. The presence of preformed DSAs can lead to immediate hyperacute rejection, while the development of de novo DSAs in previously nonsensitized patients is linked to late acute antibody-mediated rejection and chronic antibody-mediated rejection. The characteristics of DSAs, such as HLA classes and IgG subclasses, play a significant role in determining the clinical outcomes of transplant patients. Integrating complement binding and IgG subclass assays into risk assessment can significantly reduce the risk of antibody-mediated rejection and graft loss.
Doctors recommend routine monitoring of donor-specific antibodies at three to six months after transplantation and then every year. Regular testing helps identify patients at risk for antibody-mediated rejection. Early detection allows for timely intervention and better graft survival.
Laboratory and Clinical Assessment
Doctors use laboratory and clinical assessment tools to improve diagnosis of specific antibody deficiency and antibody-mediated rejection. These tools help establish diagnostic criteria and guide treatment decisions. The Pleximmune test is the only FDA-approved blood test for predicting rejection in pediatric liver or intestine transplant recipients. This test shows high sensitivity and specificity, which helps doctors manage immunosuppression and lower the risk of infection.
- Pleximmune test predicts rejection in pediatric transplant recipients.
- Sensitivity and specificity approach or exceed 80%.
- Helps manage immunosuppression and reduce infection risk.
Doctors also measure immunoglobulin levels, IgG subclass levels, and specific antibody responses. These tests confirm defective antibody production, even when total immunoglobulin levels appear normal. Evaluation of spontaneous antibodies and immunization response assessment provide more information about the patient’s immune system. Neoantigen vaccination helps assess humoral immune response in patients receiving immunoglobulin therapy.
| Assessment Tool | Description |
|---|---|
| Immunoglobulin levels | Measure levels of IgG, IgA, IgM, and IgE to assess antibody-mediated immune function. |
| IgG subclass levels | Useful for evaluating IgA-deficient patients with recurrent infections. |
| Specific antibody responses | Confirms defective antibody production, especially when total immunoglobulin levels are normal. |
| Evaluation of spontaneous antibodies | Checks for anti-blood group antibodies and responses to previous immunizations or infections. |
| Immunization response assessment | Measures antibody levels pre- and post-immunization to evaluate in vivo antibody production. |
| Neoantigen vaccination | Assesses humoral immune response in patients on immunoglobulin therapy, available in specialized centers. |
Doctors face challenges in diagnosing antibody-mediated rejection in patients with specific antibody deficiency. Invasive biomarker sampling can vary and often occurs when the disease is advanced. The clinical relevance of donor-specific antibodies detected by sensitive assays remains unclear. Biomarkers require independent validation before doctors can rely on them for diagnosis.
| Challenge | Description |
|---|---|
| Variability in Invasive Biomarker Sampling | Invasive biomarkers are crucial for accurate diagnosis but suffer from variability in sampling and interpretation, often used when the disease is advanced. |
| Unclear Clinical Relevance of DSAs | While Luminex bead assays enhance DSA detection sensitivity, their clinical significance in predicting ABMR onset or allograft survival is uncertain. |
| Need for Independent Validation | The implementation of biomarkers in clinical settings necessitates thorough independent validation to ensure reliability. |
Doctors emphasize the importance of regular monitoring for donor-specific antibodies and complement-binding antibodies. This approach helps reduce the risk of antibody-mediated rejection and supports better graft outcomes.
Antibody-Mediated Rejection Treatment
Immunoglobulin Therapy
Immunoglobulin therapy remains a key part of antibody-mediated rejection treatment in patients with specific antibody deficiency. Doctors use intravenous immunoglobulin to provide extra antibodies. This therapy helps control infections and supports the immune system when the body cannot make enough antibodies on its own. Immunoglobulin therapy can also lower the levels of harmful antibodies that attack the transplanted organ. Many transplant teams choose this treatment of antibody-mediated rejection because it improves graft survival and reduces the risk of infection.
Doctors often combine immunoglobulin therapy with other treatments for antibody-mediated rejection. They monitor patients closely to adjust the dose and timing. This approach helps maintain the right balance between fighting infection and preventing antibody-mediated injury to the graft. Immunoglobulin therapy works best when started early, before severe antibody-mediated damage occurs.
Immunosuppression Adjustments
Immunosuppression adjustments play a major role in the treatment of amr. Doctors use several drugs to target the cells that produce antibodies. Mycophenolate mofetil acts as a metabolic inhibitor and reduces the activity of B cells, which make antibodies. Rituximab, an antibody-directed therapy, depletes B cells directly. Eculizumab blocks the C5 complement protein, stopping the complement pathway that leads to antibody-mediated injury. Bortezomib targets plasma cells, which are responsible for producing large amounts of antibodies.
Doctors often use a combination of these therapies for the treatment of amr. They tailor the plan to each patient’s needs. Multidisciplinary care teams—including transplant specialists, immunologists, and pharmacists—work together to monitor antibody levels and adjust medications. This individualized approach helps prevent further antibody-mediated rejection and supports long-term graft health.
Tip: Early and regular monitoring of antibody levels allows doctors to adjust the treatment of amr quickly, reducing the risk of severe antibody-mediated injury.
New therapies continue to emerge for antibody-mediated rejection treatment. Doctors hope these advances will improve outcomes for patients with specific antibody deficiency and reduce the risk of graft loss.
Future Directions
Research Priorities
Researchers continue to search for new ways to improve outcomes in transplantation. They focus on antibody-mediated rejection and the risk it poses to graft survival. Many teams study heart transplantation and how antibody responses affect long-term results. Scientists test new drugs to lower the risk of antibody-mediated injury. Recent advancements in graft-versus-host disease treatment include the approval of ibrutinib, belumosudil, and ruxolitinib. Large trials show ruxolitinib works better than older therapies for both acute and chronic cases. Investigators also explore IL-22, R-spondin, and glucagon-like peptide-2. Cellular therapies, such as mesenchymal stem cells and regulatory T cells, may help reduce antibody-mediated damage and improve graft survival.
Researchers believe that intravenous immunoglobulin can lower anti-HLA antibody levels. This approach allows more patients to receive a transplant, even those with high antibody risk. It also improves outcomes for heart transplantation and other organ transplants.
Improving Graft Survival
Doctors use several strategies to improve graft survival in patients with specific antibody deficiency. They monitor antibody levels and adjust treatments to lower the risk of antibody-mediated rejection. Heart transplantation teams focus on early detection of donor-specific antibodies. They use high dose intravenous immunoglobulin alone or combine it with plasma exchange and rituximab. These therapies help control antibody-mediated injury and support long-term graft health.
| Treatment Strategy | Graft Survival Rate (%) | Duration (Months) |
|---|---|---|
| High dose IVIG alone | 89.1 | 24 |
| Combined therapy (IVIG + PP + rituximab) | 91.7 | 36 |
| High dose IVIG alone (monotherapy) | 50 | 36 |
Transplant teams teach patients about the risk of antibody-mediated rejection. They encourage regular follow-up and testing after heart transplantation. Doctors believe that new therapies and better monitoring will lower the risk of graft loss. Researchers continue to study antibody responses and develop new treatments for transplantation. These efforts aim to improve graft survival and reduce the risk of antibody-mediated injury for all transplant patients.
Specific antibody deficiency increases the risk of antibody-mediated complications after heart transplantation. Early detection of donor-specific antibody improves outcomes, as shown in the table below:
| Evidence Type | Description |
|---|---|
| Early Detection of DSA | Early detection of donor-specific HLA antibody links to a 3.3-fold higher risk of antibody-mediated rejection. |
| Risk Factors | Patients with HLA sensitization show a higher risk for early antibody detection. |
| Outcomes | The presence of antibody at any time after heart transplantation remains a consistent risk for worse graft outcomes. |
Transplant teams use immunoglobulin replacement therapy and follow strict vaccination protocols to manage antibody-mediated risk. They monitor immune reconstitution and maintain specific IgG levels. Long-term therapy may be needed for some patients. Clinicians stay alert for humoral dysfunction, especially in those with higher risk. Multidisciplinary collaboration improves diagnostic accuracy and management of antibody-mediated rejection. Standardized care and input from specialists help address the risk of antibody-mediated injury in heart transplantation. Ongoing research and teamwork support better outcomes for patients facing antibody-mediated risk after heart transplantation.
FAQ
What is a risk factor for chronic lung allograft dysfunction?
A risk factor for chronic lung allograft dysfunction includes the presence of donor-specific antibodies. These antibodies can damage the transplanted lung over time. Doctors monitor patients closely to reduce this risk and improve long-term outcomes.
How do doctors diagnose pulmonary AMR?
Doctors use blood tests and tissue samples for the diagnosis of pulmonary amr. They look for donor-specific antibodies and signs of injury in the lung tissue. Early diagnosis helps guide treatment and protect the graft.
What causes antibody-mediated endothelial injury?
Antibody-mediated endothelial injury happens when antibodies attack the lining of blood vessels in the transplanted organ. This injury can lead to inflammation and graft rejection. Doctors watch for this problem to prevent long-term damage.
Why is immunosuppressive therapy important after transplantation?
Immunosuppressive therapy helps stop the immune system from attacking the transplanted organ. These medicines lower the chance of rejection and keep the graft working well. Doctors adjust the therapy to fit each patient’s needs.
What is a common risk factor for transplant rejection?
A common risk factor is the development of donor-specific antibodies. These antibodies can trigger immune responses that harm the transplanted organ. Regular monitoring helps doctors catch problems early.