News & Events
Mastering T Pallidum Antibody Testing Methods for Reliable Results
Accurate detection of t pallidum antibodies shapes the success of syphilis diagnosis and treatment. You face a growing challenge as the number of new syphilis cases rises worldwide.
- The global number of syphilis cases increased from about 8.8 million in 1990 to over 14 million in 2019.
- In 2021, there were around 20.48 million people living with syphilis.
Doctors often call syphilis the “great imitator” because it can look like many other diseases. You may see unclear test results, especially in patients who have other infections. This makes it important to understand both traditional and modern testing methods.
Key Takeaways
- Start syphilis screening with a sensitive treponemal test like EIA or CIA. This helps detect early infections effectively.
- Use nontreponemal tests such as RPR to check for active syphilis. These tests indicate if the infection is currently present.
- Combine different tests for accurate diagnosis. Relying on one test can lead to misdiagnosis, so always confirm results with a second method.
- Monitor nontreponemal test titers after treatment. A fourfold decrease in titers within 6 to 12 months indicates successful therapy.
- Stay updated with CDC guidelines and new testing methods. Continuous learning improves patient outcomes and ensures reliable results.
T Pallidum Antibodies
Types of Antibodies
When you encounter syphilis, your immune system reacts by producing two main types of t pallidum antibodies. The first group, called nontreponemal antibodies, forms in response to damage caused by the infection. These antibodies react to lipids from both your own cells and the membrane of treponema pallidum. Nontreponemal antibodies often appear during active syphilis and can disappear after treatment. The second group, treponemal antibodies, targets specific proteins found only in treponema pallidum. These antibodies stay in your body for life, even after you finish treatment.
The presence or absence of these t pallidum antibodies helps you understand the stage of syphilis. Nontreponemal antibodies usually show up when the infection is active. Treponemal antibodies confirm that you have been exposed to treponema pallidum at some point, even if the infection is no longer active.
Note: Your immune system uses both humoral and cellular responses to fight treponema pallidum. Macrophages help clear the bacteria by using antibodies to mark them for destruction.
| Evidence | Description |
|---|---|
| Immune Response Mechanism | The immune response to treponema pallidum involves both humoral and cellular mechanisms, influencing the production of non-treponemal and treponemal antibodies. |
| Antibody Types | Non-treponemal antibodies react to damaged host cells and lipids from the bacterial membrane, while treponemal antibodies specifically target treponema pallidum proteins. |
| Role of DTH | The effectiveness of the delayed-type hypersensitivity (DTH) response is crucial in determining the course of the disease and the types of antibodies produced. |
Detection Methods
You have several options for the detection of t pallidum antibodies. Serological tests play a key role in diagnosing syphilis. Nontreponemal tests, such as VDRL and RPR, detect antibodies that signal active infection. Treponemal tests, like FTA-ABS and TPHA, confirm exposure to treponema pallidum by finding antibodies specific to the bacterium.
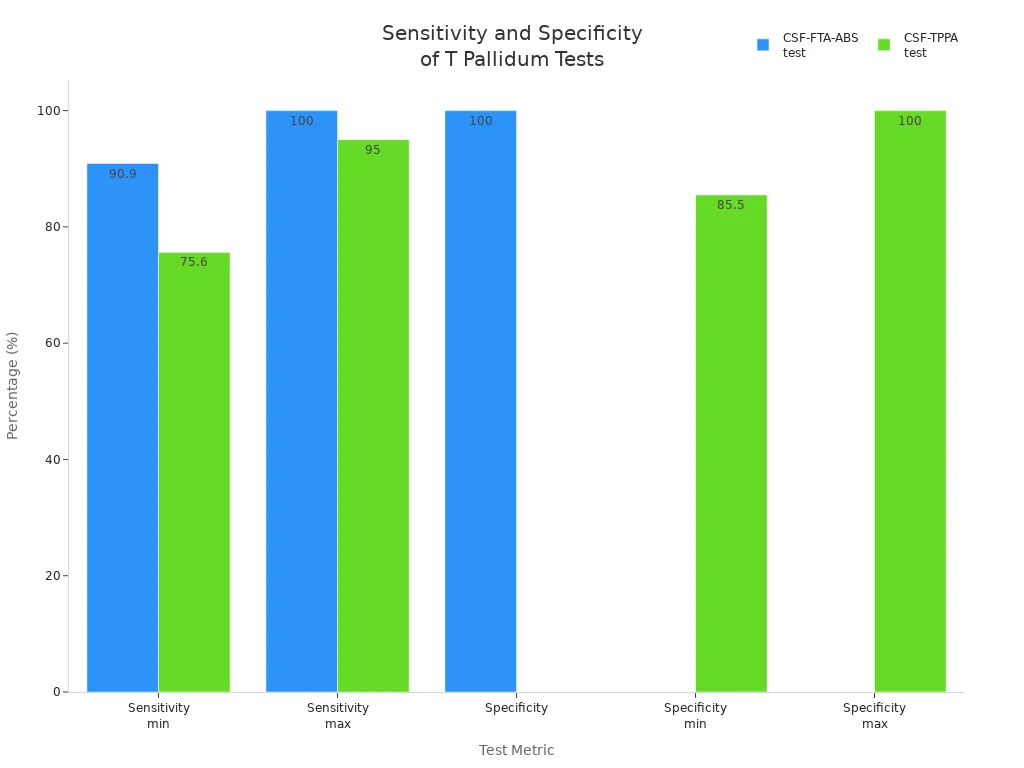
Modern detection methods include PCR and chemiluminescence immunoassays (CLIAs). PCR can detect treponema pallidum DNA in lesions, but its sensitivity varies. For example, the T. pallidum PCR test for primary lesions shows a sensitivity of 75%–95% and a specificity of 97%–100%. The CSF-FTA-ABS test, used for neurosyphilis, has a sensitivity of up to 100% and a specificity of 100%.
You should also consider turnaround time and cost-effectiveness. CLIAs are both cost-effective and fast. The BioPlex syphilis IgG assay can process 100 samples in just 1.75 hours, while other tests may take longer. Screening with RPR is inexpensive, but it may miss many true cases.
By understanding these detection methods, you can choose the best test for each patient and improve the accuracy of syphilis diagnosis.
Laboratory Techniques

Serological Tests
You rely on serology as the main approach for diagnosing syphilis. Serological testing helps you detect antibodies that your body produces in response to treponema pallidum. These tests fall into two main groups:
- Nontreponemal tests look for antibodies against cardiolipin-lecithin-cholesterol antigens. These antigens are not unique to treponema pallidum, so these tests can sometimes give false positives.
- Treponemal tests detect antibodies that target specific parts of treponema pallidum. These tests offer higher specificity and reduce the chance of false positives.
You use nontreponemal tests like VDRL and RPR to screen for syphilis and to measure disease activity. Treponemal tests such as FTA-ABS, TP-PA, CIA, and EIA confirm the diagnosis after a positive screening result.
Recent studies show that treponemal antibody tests, once thought to have very low false-positive rates, now show a higher number of unconfirmed positive results. This means you must interpret results carefully and consider the clinical context.
Serology remains the backbone of syphilis diagnostic work. You should remember that no single test is perfect. Combining different serological tests improves accuracy and helps you avoid misdiagnosis.
Direct Detection Methods
Direct detection methods allow you to find treponema pallidum in patient samples without relying on antibodies. These methods include antigen detection and nucleic acid amplification. You use them mostly in early syphilis when serology may not yet show positive results.
| Method | Stage of Syphilis | Sensitivity (%) | Specificity (%) |
|---|---|---|---|
| TmpA | Primary | 98.7 | 100 |
| TmpA | Secondary | 97.4 | 100 |
| TmpA | Early Latent | 83.6 | 100 |
| TpN17 | Primary | 100 | 100 |
| TpN17 | Secondary | 100 | 100 |
| TpN17 | Early Latent | 93.2 | 100 |
| TmpA ELISA | Primary | 76 | N/A |
| TmpA ELISA | Secondary | 100 | N/A |
| TmpA ELISA | Early Latent | 98 | N/A |
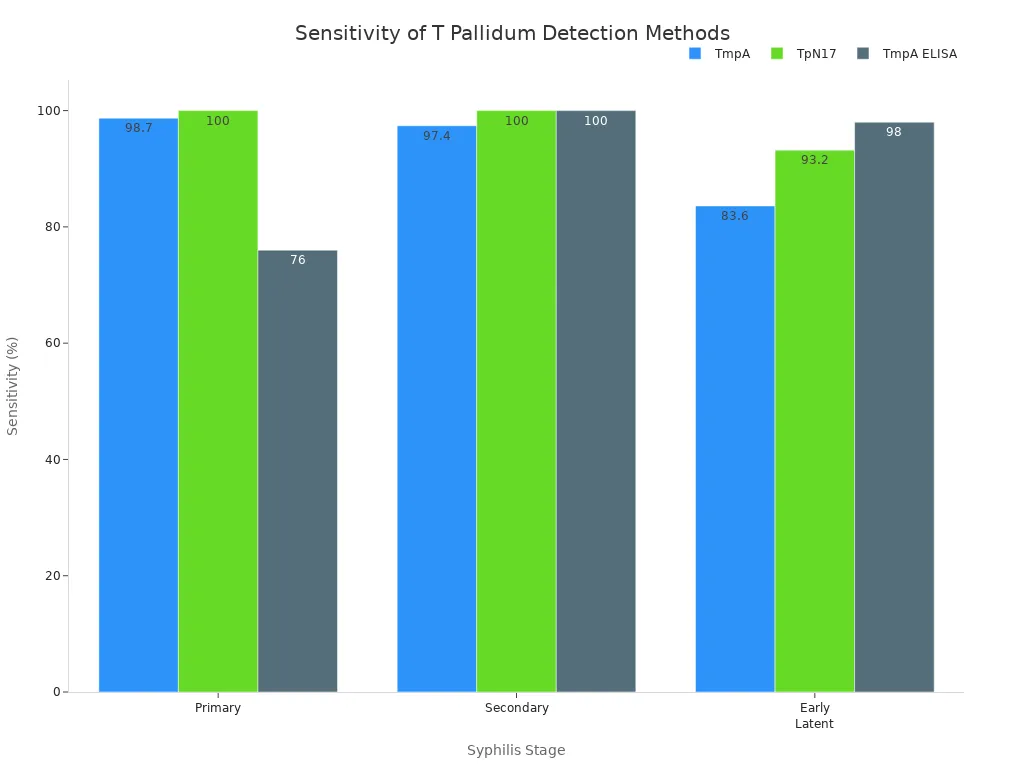
The main limitations of direct detection methods include the need for skilled personnel, special reagents, and advanced equipment. Some older methods, like the rabbit infectivity test, are no longer used because they are time-consuming and raise ethical concerns. Microscopy is less common now due to its subjectivity and technical demands. Nucleic acid amplification tests still face challenges with sample types and DNA extraction.
You should use direct detection methods when you need fast and specific answers, especially in early or unclear cases. However, you must understand their limitations and always interpret results alongside serology and clinical findings.
Testing Algorithms
Traditional Algorithm
You may know the traditional algorithm as the classic approach for diagnosing syphilis. This method starts with a nontreponemal test, such as the RPR. If you get a positive result, you confirm it with a treponemal test. The Centers for Disease Control and Prevention (CDC) recommends this approach for initial syphilis screening. Many clinical laboratories use it because it fits well with their workflow and keeps costs low. Smaller labs often choose this method since it works best when you have fewer samples to process.
The traditional algorithm usually produces fewer false positives than newer methods. It works well in populations where most people have not had syphilis before. In these groups, you will likely find more true positive cases. However, this method can miss early or latent syphilis, especially in areas where the disease is common. Studies show that the traditional algorithm may not detect some cases that newer methods can find.
Reverse Sequence Algorithm
The reverse sequence algorithm changes the order of testing. You start with a treponemal test, such as EIA or CIA. If you get a positive result, you follow up with a nontreponemal test. Recent studies show that this approach finds more cases of syphilis, especially in early and latent stages. For example:
- The reverse sequence algorithm detects a higher seroprevalence of syphilis (62.4%) compared to the traditional algorithm (40.8%).
- The traditional algorithm misses about 34.6% of cases.
- The false-positive rate drops from 6.8% with the traditional method to only 0.6% with the reverse sequence.
- The reverse sequence is better at finding hidden or early infections.
However, you may see more discordant results with the reverse sequence algorithm. The table below shows how often this happens in different populations:
| Population Prevalence | EIA/CIA Reactive Rate | Discordant Results Rate | Nonreactive TP-PA/FTA-ABS Rate |
|---|---|---|---|
| High | 14.5% | 50.6% | 14.1% |
| Low | 2.3% | 60.6% | 40.8% |
Tip: Choose your algorithm based on your lab’s resources, the population you serve, and the stage of syphilis you want to detect. Always confirm unexpected results with a second type of test.
Result Interpretation

Understanding how to interpret your results is essential for reliable syphilis diagnosis. You need to look at both titer changes and discordant results to make the best decisions for your patients. This section will guide you through common and complex scenarios, helping you troubleshoot and clarify confusing results.
Titer Changes
When you monitor syphilis, you often use nontreponemal test titers to track disease activity and treatment response. These titers show how much antibody is present in the blood. After treatment, you expect the titers to drop. A fourfold decline in nontreponemal antibody titers within 6 to 12 months usually means the therapy worked well. You should check titers at 6, 12, and 24 months after treatment. For early syphilis, you may also check at 3 and 9 months.
| Baseline RPR Titer | Likelihood of Serological Cure | Study Findings |
|---|---|---|
| ≤1:2 | Higher likelihood | Tong et al. |
| ≥1:64 | Higher likelihood | Tong et al. |
| >1:32 | >6-fold higher probability | HIV-negative patients with early-stage syphilis |
| 1:32 vs 1:8 | Statistically significant difference, P < 0.01 | Baseline and 6-month follow-up |
| Primary Syphilis | Higher likelihood of cure | General trend |
| Secondary/Early Latent Syphilis | 43% to 58% achieved serofast status after 6 months | General trend |
| HIV-positive patients | Lower AOR (0.32) for serological cure | Compared to primary/secondary syphilis |
You may see different titer patterns based on the stage of syphilis and the patient’s immune status. For example, HIV-positive patients often have a lower chance of serological cure. Some patients, especially those with secondary or early latent syphilis, may remain serofast, meaning their titers do not drop as expected even after successful treatment.
Tip: Always compare the baseline titer with follow-up results. A fourfold drop is a good sign. If titers do not fall, or if they rise again, you should consider possible reinfection or treatment failure.
You can use the following table to compare the sensitivity and specificity of different tests. This helps you choose the right test for each stage and situation.
| Test Type | Sensitivity | Specificity |
|---|---|---|
| TPPA | 96.25% | 98.38% |
| TP-ELISA | 100% | 95.41% |
| TP-CMIA | 100% | 94.86% |
| RPR | 73.13% | 86.22% |
| TRUST | 73.75% | 86.49% |
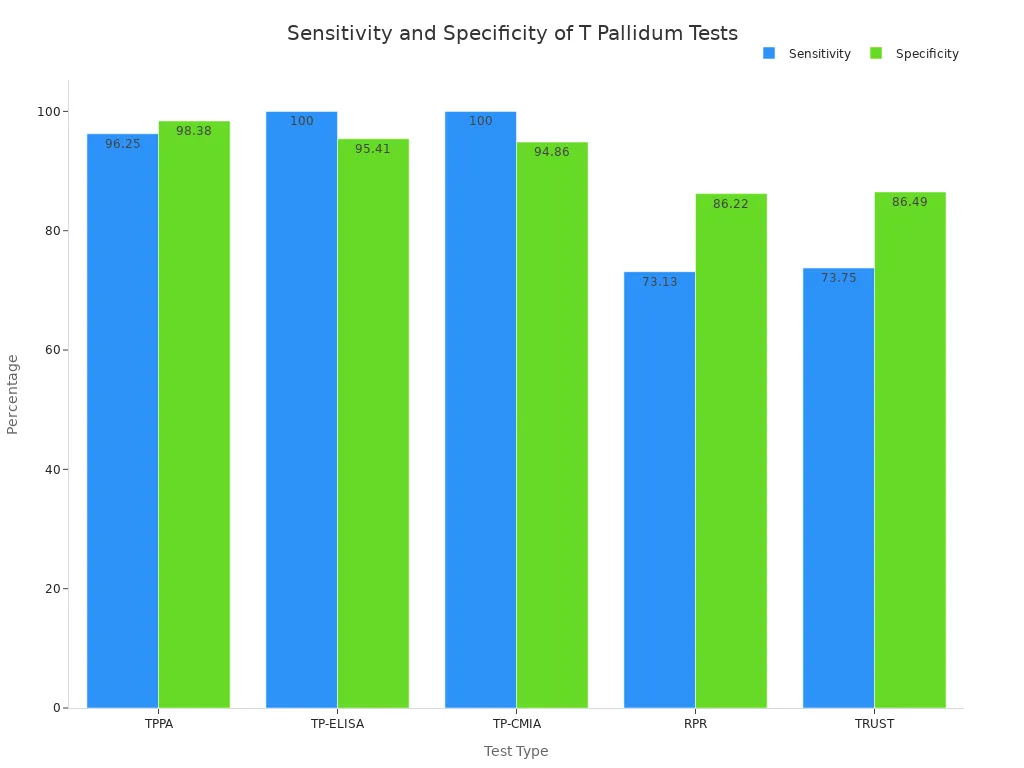
You should remember that treponemal tests like TPPA, TP-ELISA, and TP-CMIA are best for routine screening. Nontreponemal tests such as RPR and TRUST are better for monitoring therapy response. Always tailor your choice of test to the clinical needs of your patient.
Discordant Results
You may sometimes see results that do not match. Discordant results happen when one test is positive and another is negative. This can make syphilis diagnosis more difficult. You need to know the most common causes and how to handle these situations.
- Over half of reactive EIA or CIA results are nonreactive by RPR.
- About one-third of these are also nonreactive with a confirmatory treponemal test.
- Discordant samples are more common in low-prevalence populations.
- Past treated syphilis can cause treponemal tests to stay positive for life.
- Early primary syphilis may show positive treponemal results before nontreponemal results appear.
- False-positive EIA or CIA results can occur in low-risk groups.
To minimize errors in interpreting T. pallidum antibody test results, you should use a combination of serologic tests, follow CDC guidelines for confirmatory testing, and always correlate results with clinical history and symptoms.
The traditional algorithm for diagnosing syphilis starts with a screening nontreponemal test, such as the RPR, and verifies positive results with a confirmatory treponemal test, such as fluorescent treponemal antibody absorption (FTA-ABS) or T. pallidum particle agglutination assay (TP-PA). However, this algorithm often misses early primary syphilis since the RPR can take up to four weeks to become positive and can also fail to identify latent or tertiary disease because antibody levels wane over time.
When you face discordant results, follow these troubleshooting steps:
- Review the patient’s history for previous syphilis diagnosis or treatment. If the patient was treated and has no new risk, the results may reflect past infection.
- If the patient is untreated, start therapy for syphilis, usually with penicillin-G injections for late latent cases.
- If you suspect early primary syphilis and see a painless sore but negative nontreponemal results, repeat the test in 12–14 days and consider starting treatment.
- Watch for the prozone reaction, which can cause false negatives in secondary syphilis. Ask the lab to dilute the sample if clinical suspicion remains high.
You may also see false positives, especially in low-prevalence areas. In these cases, negative RPR and TPPA confirmation suggest the initial positive was not true. If you suspect immunodeficiency, remember that serology tests may be falsely negative.
- If you suspect early acute primary syphilis, repeat testing in 12–14 days.
- Serology tests may be falsely negative in patients with immunodeficiency.
- Syphilis total antibodies can have false positives, indicated by negative RPR and TPPA confirmation.
- In low-prevalence areas, false positives make up a significant part of positive screening results.
Note: Always use clinical judgment and consider the whole picture, including symptoms and risk factors, when interpreting results.
You can use this simple flowchart to help guide your interpretation of discordant results:
If Treponemal Test Positive and Nontreponemal Test Negative:
- Check for past syphilis treatment.
- If untreated, consider early infection or false positive.
- Repeat nontreponemal test in 2 weeks.
- If symptoms present, treat empirically.
If Both Tests Positive:
- Diagnose active syphilis.
- Start treatment and monitor titers.
If Both Tests Negative:
- No evidence of syphilis.
- If high suspicion, repeat testing in 2 weeks.
By following these steps, you can improve the accuracy of your results and provide better care for your patients. Always remember to use a combination of tests, follow guidelines, and consider the clinical context for every syphilis diagnosis.
You can master T pallidum antibody testing by following key steps:
- Start with a sensitive treponemal test, such as EIA or TP-PA.
- Use a non-treponemal test like RPR to check for active infection.
- Add a second treponemal test if results do not match.
Selecting the right laboratory methods improves patient outcomes, including a 79.2% serological cure rate at 12 months. Keep learning and follow CDC guidelines to stay current with new testing methods and ensure reliable results.
FAQ
What is the best first step for syphilis screening?
You should start with a sensitive test, such as EIA or CIA, for syphilis screening. These tests help you find early infections. Always confirm positive results with another method to make sure your screening is accurate.
How often should you repeat screening for syphilis?
You should repeat screening every 3 to 6 months if you have a high risk. For most people, yearly screening is enough. Regular screening helps you catch new infections early and protect your health.
Why do some screening tests give false positives?
Screening tests can react to other conditions, such as autoimmune diseases or pregnancy. This can cause false positives. You should always confirm positive screening results with a second, more specific test.
Can you rely on one screening test for diagnosis?
You should not rely on a single screening test. Combining different tests gives you more reliable results. This approach helps you avoid mistakes and ensures you get the right diagnosis.
What should you do if your screening results do not match?
If your screening results do not match, review your medical history and risk factors. Repeat the tests after two weeks. You may need to use a different method or consult a specialist for help.